By Dr. Niraj Ghanghoriya, Dental Specialist | ToothCareUSA.com
Introduction
Welcome to ToothCareUSA.com. In my daily practice as a dental specialist, I often find that the biggest hurdle in treating gum disease isn’t the procedure itself—it’s the lack of understanding about the condition. Many patients believe that a little bleeding when flossing is normal. It is not.
Gum disease is a silent, progressive infection that doesn’t just threaten your teeth; it can impact your overall systemic health. My goal with this guide, and the accompanying visual aids from our Pinterest boards, is to empower you with the knowledge to recognize the signs early. Knowledge is the first step toward saving your smile. Let’s explore exactly what is happening beneath the gumline.
What is periodontal disease?
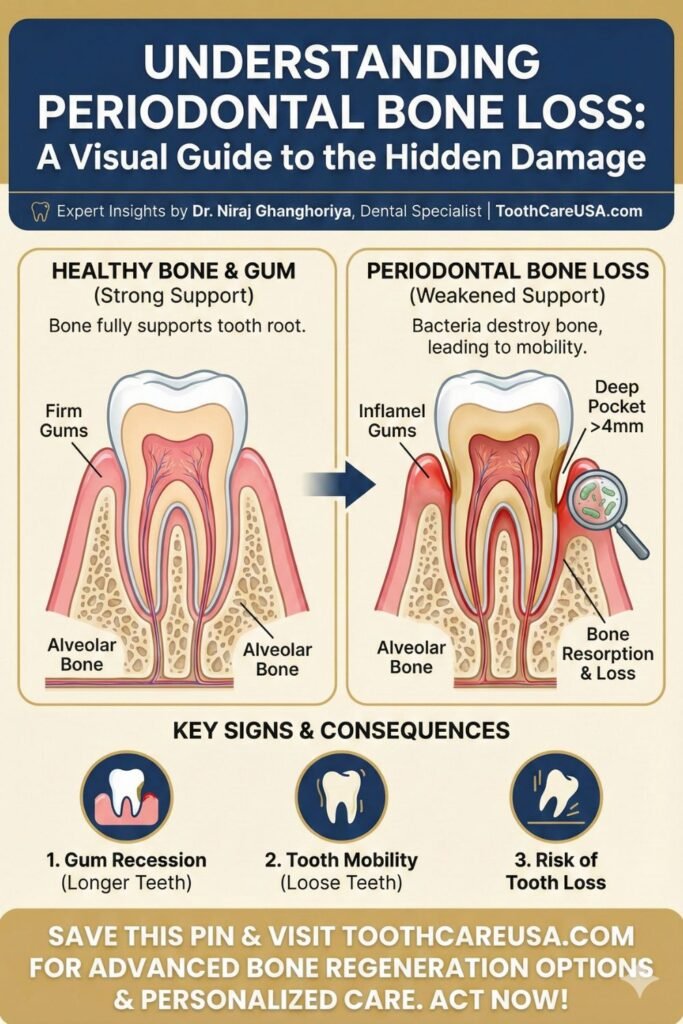
“Periodontal” literally means “around the tooth.” Therefore, periodontal disease is a chronic inflammatory condition that affects the tissues surrounding and supporting your teeth. This includes the gingiva (gums), the periodontal ligament, and the alveolar bone (the jawbone that holds the tooth sockets).
It is crucial to understand that this is not just a “tooth problem”; it is a bacterial infection. When bacteria in your mouth form a sticky film called plaque, and that plaque is not adequately removed, it hardens into tartar (calculus). This buildup harbors bacteria that release toxins, triggering your body’s immune system. Unfortunately, the resulting inflammation—your body’s attempt to fight the invaders—ends up destroying the very gum and bone tissue that supports your teeth.
According to the Centers for Disease Control and Prevention (CDC), nearly half (47.2%) of adults aged 30 years and older have some form of periodontal disease. That number increases to over 70% for adults 65 and older. Despite these high numbers, many people are unaware they have it because the early stages are often painless.
In my clinical experience, the biggest misconception patients have is that if nothing hurts, nothing is wrong. Periodontal disease is often a “silent killer” of teeth. By the time you feel significant pain or notice a tooth is loose, the disease is usually in an advanced stage where damage is irreversible.
Dr. Niraj’s Clinical Advice: Think of your teeth like a house and your gums and bone as the foundation. You can have a beautiful house, but if the foundation is crumbling due to an unchecked infection, the house will eventually fall. Treating cavities without addressing gum disease is like painting the walls while the foundation cracks.
Periodontal Disease
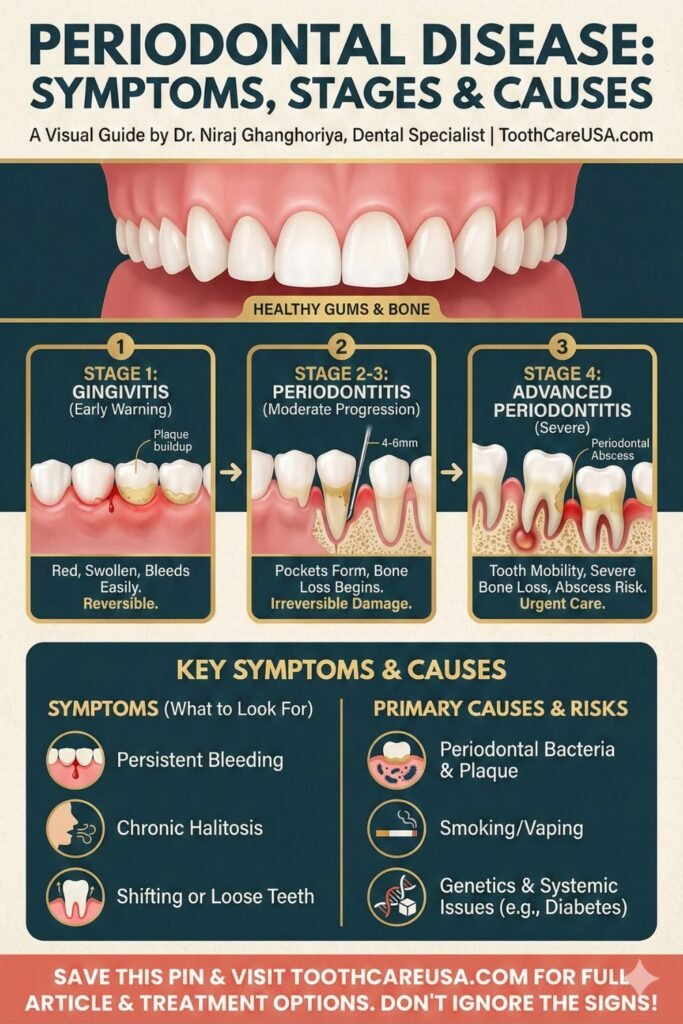
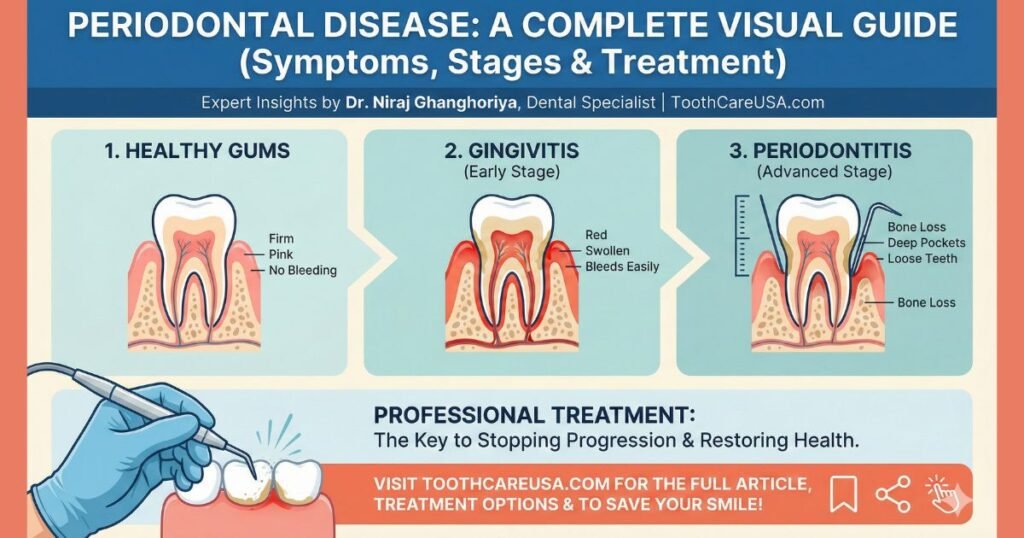
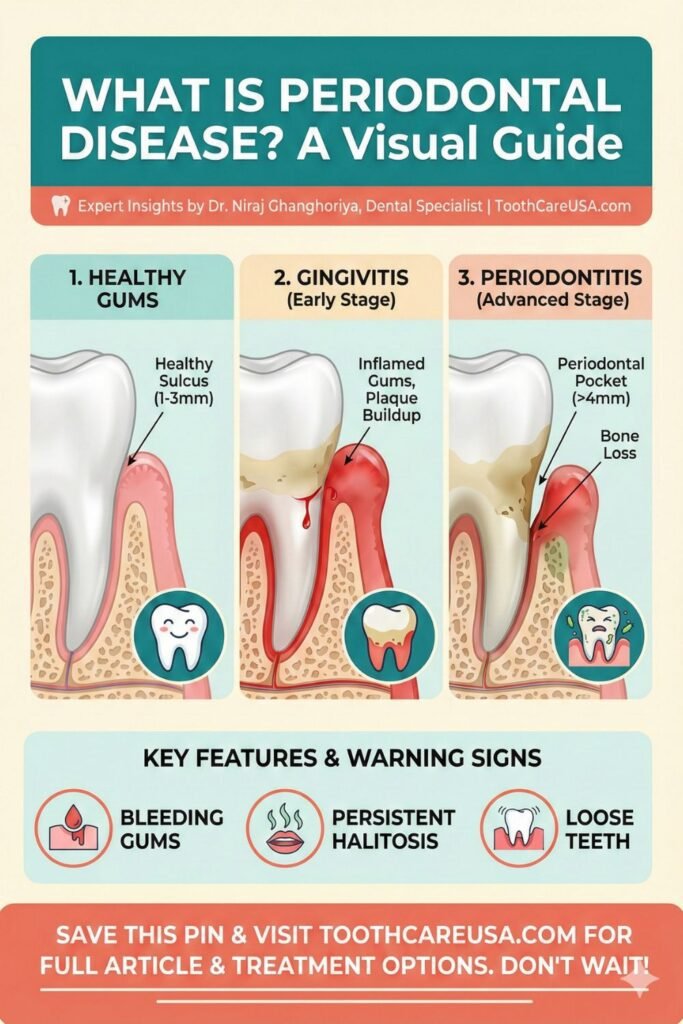
When we use the broad term “periodontal disease,” we are describing a spectrum of conditions ranging from mild inflammation to severe tissue destruction. It is generally categorized into two major phases: gingivitis and periodontitis.
Gingivitis is the earliest and mildest form of periodontal disease. It is caused by plaque buildup at the gumline, leading to inflammation. The key symptoms here are gums that are red, swollen, and bleed easily during brushing or flossing. The critical takeaway about gingivitis is that it is reversible. With professional cleaning and improved at-home oral hygiene, the gums can return to a healthy state.
If gingivitis is left untreated, it can advance to periodontitis. At this stage, the inflammation has spread below the gumline, and the inner layer of the gum and bone pulls away from the teeth. This is where true structural damage begins. Unlike gingivitis, the bone loss associated with periodontitis is largely irreversible.
The symptoms of established periodontal disease become more visually apparent:
- Persistent Bad Breath (Halitosis): Caused by bacteria and decaying cellular matter in deep pockets.
- Gum Recession: Your teeth may appear “longer” because the gum tissue is shrinking away.
- Changes in Bite: You might notice your teeth feel different when you chew or fit together differently.
- Loose Teeth: As bone support is lost, teeth become mobile.
Often, patients will tell me, “My gums always bleed when I floss, that’s just how they are.” I have to gently correct them. Healthy tissue does not bleed when touched. Bleeding is the body’s universal SOS signal that an infection is present.
Periodontal Pocket

One of the most important diagnostic tools we use in dentistry is the periodontal probe—a tiny “ruler” that measures the space between your tooth and gum. When you hear your dentist or hygienist calling out numbers during your exam (like “3, 2, 3… 5, 4, 5”), they are measuring your periodontal pockets.
In a healthy mouth, the gum tissue fits snugly around the tooth, much like a tight turtleneck sweater around your neck. There is a shallow, natural space called a sulcus, which typically measures between 1 and 3 millimeters in depth. This depth is easy to clean with a toothbrush and floss.
However, as periodontal disease progresses and the supporting tissue is destroyed, the gum detaches from the tooth. The sulcus deepens, turning into a periodontal pocket.
- 4mm – 5mm pockets: These indicate early to moderate periodontitis. At this depth, your toothbrush bristles and floss cannot reach the bottom of the pocket to clean out the bacteria. It becomes a protected breeding ground for infection.
- 6mm+ pockets: These indicate severe disease. These deep spaces allow very aggressive, anaerobic bacteria to thrive, accelerating bone destruction.
When a patient has deep pockets, standard cleaning is no longer sufficient. The bacteria are out of reach. This is why we recommend treatments like Scaling and Root Planing (deep cleaning) to physically remove the bacterial colonies from deep within these pockets and smooth the root surface to encourage re-attachment.
Dr. Niraj’s Clinical Insight: A periodontal pocket is essentially a hidden reservoir of infection. You cannot clean a 6mm pocket at home any more than you could clean under your fingernails if you couldn’t reach them. Professional intervention is the only way to disrupt that bacterial ecosystem.
Periodontal Staging and Grading
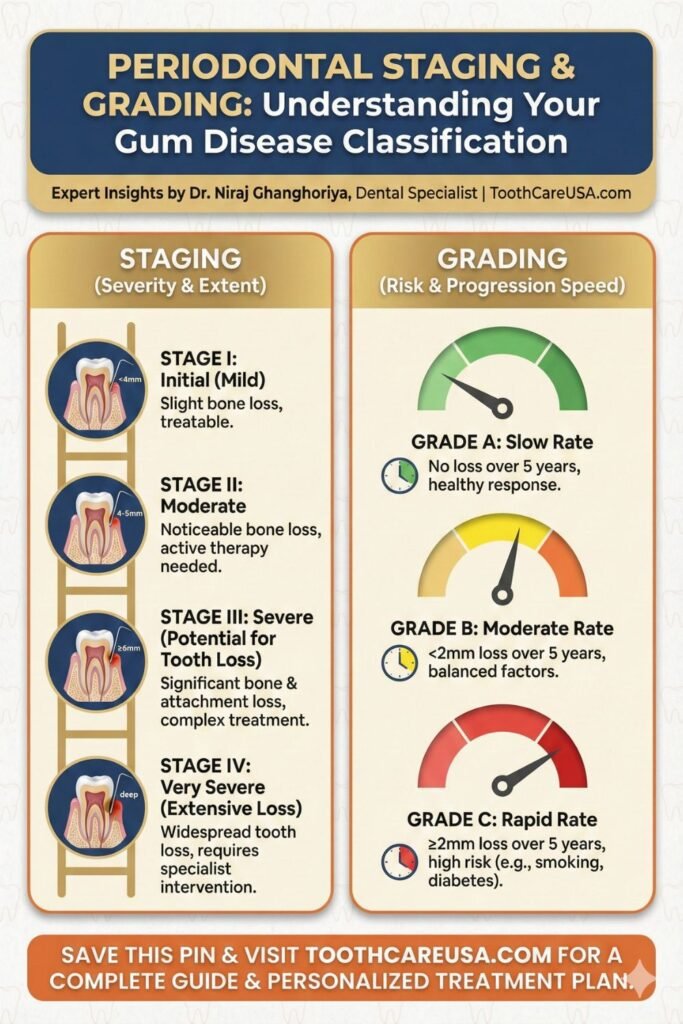
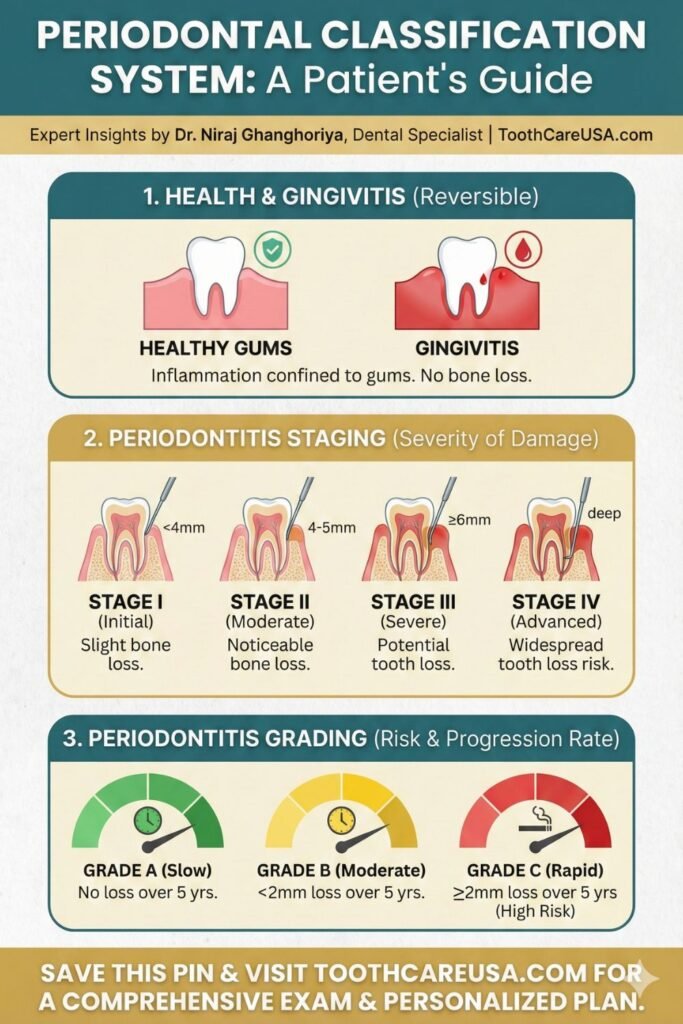
Modern dentistry moves beyond just saying you “have gum disease.” We now use a sophisticated system developed by the American Academy of Periodontology (AAP) to define your specific condition accurately. This system is known as periodontal staging and grading, and it is essentially the current periodontal classification standard. It helps us determine not just how bad the disease is now, but how fast it is likely to get worse.
Staging (How severe is the damage right now?) Staging looks at the severity of the disease based on bone loss, pocket depth, and tooth loss due to periodontitis.
- Stage I (Initial): The earliest stages of bone loss.
- Stage II (Moderate): Established bone loss, but the teeth are not yet loose.
- Stage III (Severe): Significant bone loss with potential for tooth loss. Treatment becomes more complex.
- Stage IV (Advanced): Very severe bone loss and extensive tooth loss. This stage requires advanced, multi-disciplinary rehabilitation to restore function.
Grading (What is your risk of progression?) Grading aims to estimate the future rate of disease progression and your responsiveness to standard therapy. It considers your history of bone loss alongside vital risk factors like smoking and diabetes.
- Grade A (Slow Rate): You have a low risk of rapid progression.
- Grade B (Moderate Rate): The standard progression rate if no other major risk factors are present.
- Grade C (Rapid Rate): The disease is moving quickly. This is often seen in heavy smokers, uncontrolled diabetics, or patients with a strong genetic predisposition.
Understanding your Stage and Grade is vital because a Stage II, Grade A patient needs a very different long-term care plan than a Stage II, Grade C patient.
Periodontal Bacteria
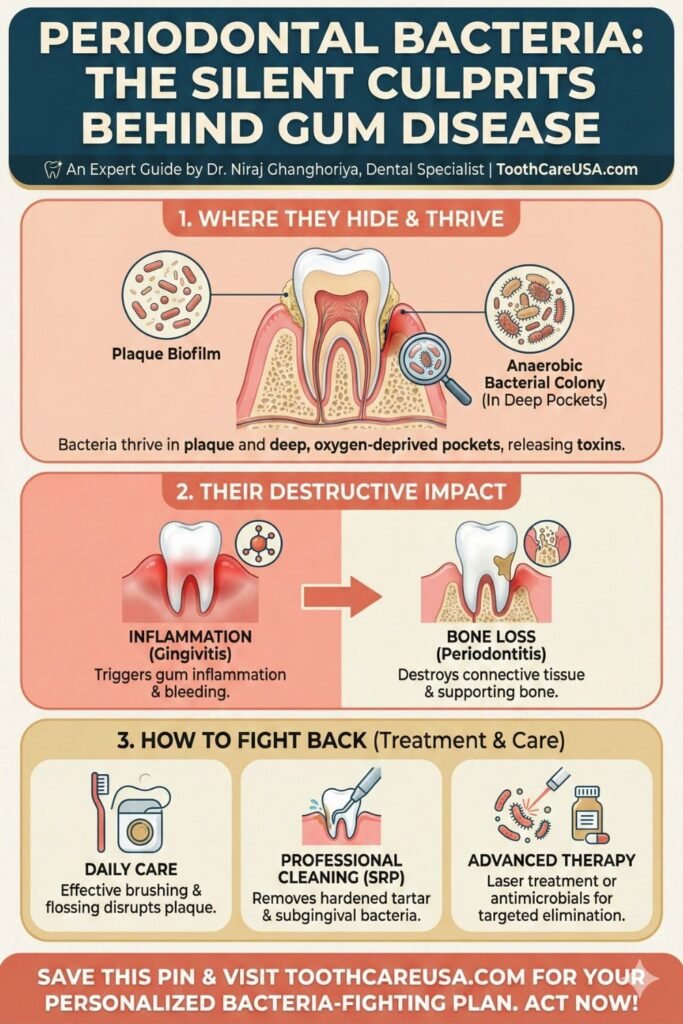
It is easy to blame sugar or “soft teeth” for dental problems, but periodontal disease is fundamentally an infectious disease caused by specific types of bacteria. The human mouth is home to hundreds of species of bacteria; most are harmless commensal bacteria, but some are highly destructive pathogens.
The primary culprits in gum disease are anaerobic bacteria. “Anaerobic” means they thrive in environments without oxygen. When your gums are healthy, oxygen-rich saliva keeps these bad bacteria in check. However, as plaque builds up and deep periodontal pockets form, the environment at the bottom of the pocket becomes oxygen-depleted. This is the perfect breeding ground for destructive bacteria.
These bacteria form a complex, organized community known as a biofilm. Within this biofilm, they communicate with each other and become highly resistant to antibiotics and the body’s immune defenses.
These pathogens do two things:
- They release toxins and enzymes that directly damage gum tissue and break down collagen.
- More significantly, their presence triggers an oversized inflammatory response from your own immune system. In a misguided attempt to kill the bacteria hidden deep in the pockets, your immune cells (like osteoclasts) end up breaking down your own jawbone.
The goal of periodontal therapy is never to sterilize the mouth—that’s impossible. The goal is to reduce the load of pathogenic bacteria below the threshold that triggers destructive inflammation, allowing the good bacteria to re-establish a healthy balance.
Periodontal Abscess
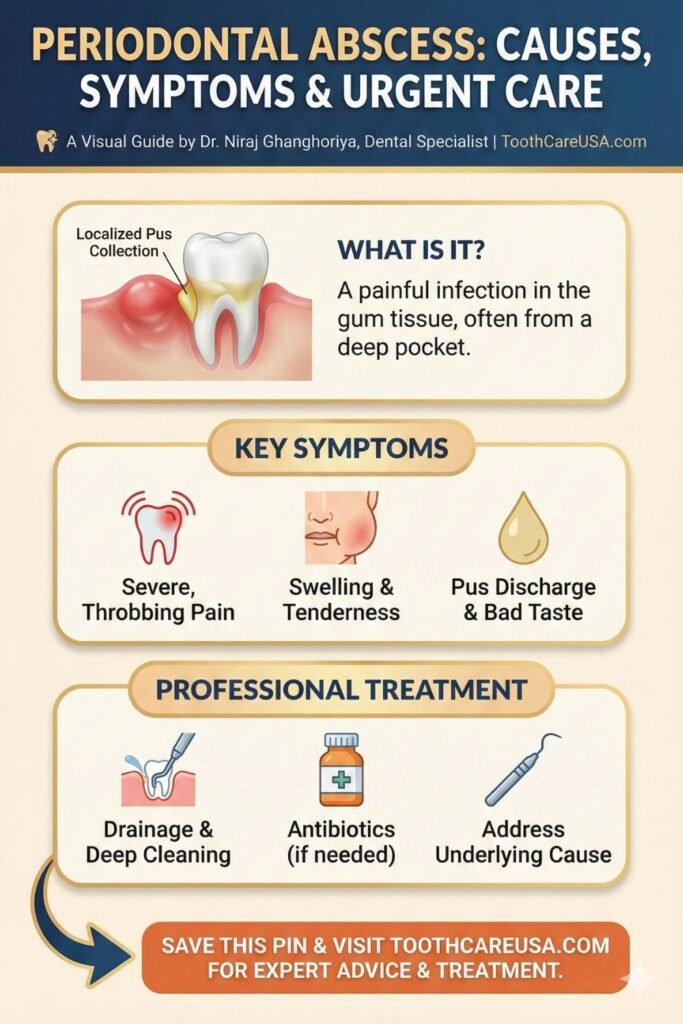
While many stages of periodontal disease are surprisingly painless, a periodontal abscess is a notable exception. This is an acute, often painful dental emergency that requires immediate professional attention.
A periodontal abscess is a localized collection of pus (an infection) within the tissues of the gum wall of a periodontal pocket. It typically happens in patients who already have existing, untreated periodontal disease.
What causes it? It usually occurs when the opening of a deep periodontal pocket becomes blocked. This can happen if food debris (like a popcorn hull or a poppy seed) gets trapped deep in the gum, or sometimes even after a partial cleaning where the gum heals tightly at the top, trapping active bacteria underneath. With nowhere to drain, the infection rapidly builds up pressure, creating a painful swelling.
Symptoms of an Abscess:
- A sudden, throbbing pain that may radiate to the ear or jaw.
- A distinct, red, swollen “bump” on the gum that looks like a pimple.
- The tooth may feel “high” when you bite down and be very tender to the touch.
- A foul taste in the mouth, especially if the abscess drains spontaneously.
Dr. Niraj’s Urgent Advice: Never attempt to pop a gum abscess yourself with a needle or sharp object. You risk spreading the infection deeper into the jaw or bloodstream. This requires professional drainage and often antibiotics to prevent systemic complications. Please call our office immediately if you notice these symptoms.
Periodontal Disease Before and After
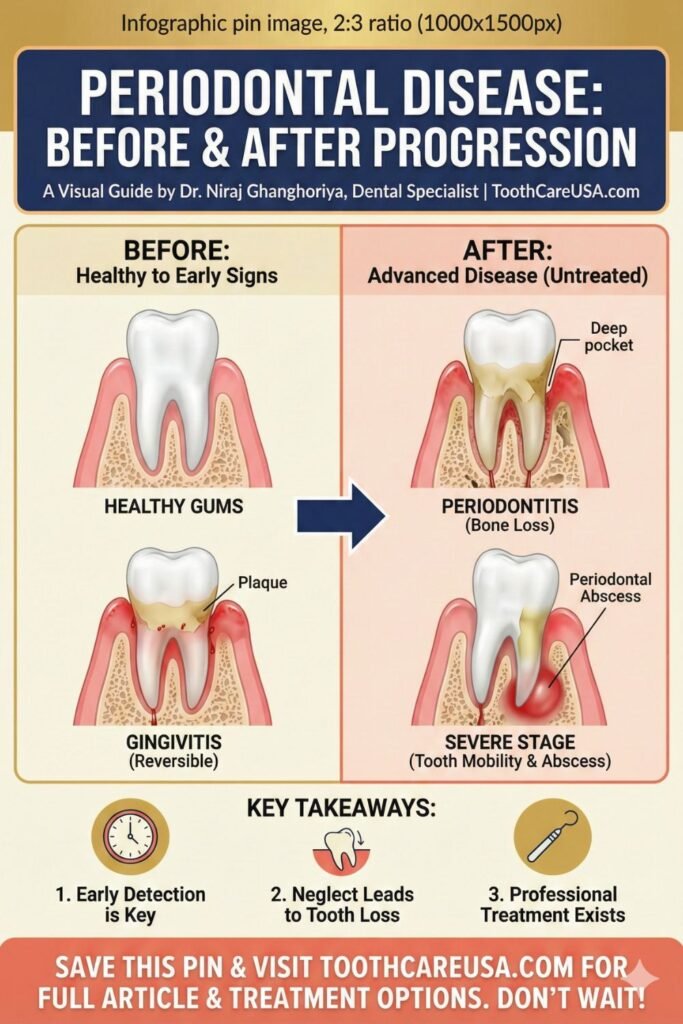
Visualizing the progression of gum disease is often the most powerful motivator for patients to accept treatment. The contrast between a healthy mouth and one ravaged by advanced periodontitis is stark.
The “Before” picture (healthy state) features knife-edged, coral-pink gums that fill the spaces between the teeth completely. The underlying bone is high and dense, holding the teeth firmly in place.
The “After” picture of untreated disease is characterized primarily by irreversible destruction. The most significant unseen change is periodontal bone loss. As the jawbone resorbs (dissolves away) due to chronic inflammation, there is less support for the teeth.
Visually, this results in:
- Longer-looking teeth: As the gum follows the receding bone, the yellowish roots of the teeth become exposed. These roots are highly sensitive to cold and sweets and are more prone to decay.
- “Black Triangles”: The small triangles of gum tissue between the teeth (papilla) are lost, leaving dark, open spaces that trap food and affect speech and esthetics.
- Splayed Teeth: Without bone support, chewing forces cause teeth to flare out, drift apart, or rotate.
The tragedy of the “After” scenario is that bone loss in the jaws does not naturally regenerate. Once it is gone, it is gone. While we have regenerative procedures (like bone grafts) that can restore some lost ground in specific defects, it is far more predictable, less invasive, and less expensive to prevent the loss in the first place.
Conclusion & Next Steps
Understanding the mechanisms of periodontal disease—from the bacteria that cause it to the staging system we use to track it—is essential for your long-term health. If you recognized any of the symptoms mentioned in this guide, or if it has been more than six months since your last comprehensive dental exam, I urge you not to wait.
Gum disease is manageable, and even reversible in its earliest stages. At ToothCareUSA.com, we are committed to helping you keep your natural teeth for a lifetime.
Disclaimer: This content is for informational purposes only and does not substitute for professional medical or dental advice, diagnosis, or treatment. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a medical condition.
References and Further Reading
- Centers for Disease Control and Prevention (CDC): Periodontal Disease Facts and Statistics. Available at: https://www.cdc.gov/oralhealth/conditions/periodontal-disease.html
- American Academy of Periodontology (AAP): Patient Resources on Gum Disease Types and Treatments. Available at: https://www.perio.org/for-patients/
- American Dental Association (ADA) MouthHealthy: Periodontitis (Gum Disease). Available at: https://www.mouthhealthy.org/all-topics-a-z/Gum-disease
FAQs On Gum Disease: Symptoms, Stages, and Causes

Can periodontal disease be cured completely?
Technically, periodontal disease (periodontitis) cannot be fully “cured” once bone loss occurs, but it can be stabilized. While the early stage, gingivitis, is 100% reversible, periodontitis is a chronic condition that requires lifelong management. In my practice, we successfully keep patients in remission for decades through consistent periodontal maintenance and excellent home care
Can lost bone from gum disease grow back?
Generally, no. Once the jawbone is destroyed by periodontal bacteria, it does not regenerate naturally on its own. The loss is permanent. However, as a dental specialist, I can sometimes use advanced regenerative procedures like bone grafting to restore specific defects. The primary goal of treatment is always to stop the progression and prevent further loss.
Is periodontal disease contagious to my partner?
Yes, the bacteria that cause gum disease can be spread through saliva via kissing or sharing utensils. However, transmission of bacteria does not guarantee your partner will develop the disease. In my clinical experience, whether the disease takes hold depends more on the individual’s own immune response, oral hygiene habits, and genetic susceptibility than just exposure alone.
How fast does gum disease progress to tooth loss?
The rate of progression varies significantly and is classified by your “Grade” (A, B, or C). For some patients, it is a slow process over decades; for others, particularly smokers or those with diabetes, “Grade C” rapid progression can destroy bone within a few years. I advise immediate treatment because we cannot always predict how aggressive your specific case will be.
What is the difference between a standard cleaning and a deep cleaning?
A standard prophylaxis cleaning only removes plaque above the gumline and is for healthy mouths. A “deep cleaning” (Scaling and Root Planing) is a therapy for periodontal disease that removes bacterial toxins from deep pockets below the gumline. I prescribe deep cleanings when pockets measure 4mm or deeper, as standard tools cannot reach these infected areas.
Periodontal Disease: Your Comprehensive Resource
I invite you to read the articles below for a complete breakdown of gum disease causes, clinical treatments, and my recommended home care routines.
Dental Implant Cost Chicago: The 2026 Price Guide & Hidden Fees S1A5
Author: Dr. Niraj Ghanghoriya (Dental Specialist) Micro-Note: Educational purposes only. See full disclaimer below. Quick…
The Real Cost of Dental Implants in Indiana: A Specialist’s Transparent Guide (2026) S1A4
By Dr. Niraj Ghanghoriya (Dental Specialist).Educational purposes only. See full disclaimer below. Quick Answer: What…
Price for Mini Dental Implants (2026 Cost Guide & Fee Breakdown) S1A3
Author: Dr. Niraj Ghanghoriya, (Dental Specialist), Educational purposes only. See full medical disclaimer below. Quick…
The Cost of Zirconia Implants: Why ‘Cheap’ Ceramic Can Cost You Your Bone
Dr. Niraj’s Quick Answer (2026 Estimate) In the US, Cost of Zirconia Implants(single) lies between…
Bolsa Periodontal: A Multilingual Guide to Gum Care,Bolsa Periodontal(Global Periodontal Health)(Blog 6)
Author: Dr. Niraj Ghanghoriya (Dental Specialist) | Website: ToothCareUSA.com Category: Global Periodontology (International Resources) Introduction…
Decoding the Dentist’s Code: Understanding Periodontal Instruments & periodontal chart (Blog 5)
By Dr. Niraj Ghanghoriya, Dental Specialist | ToothCareUSA.com Key Takeaways: The “Numbers”: Hearing “3, 2,…

Dr. Niraj Ghanghoriya is a passionate dental surgeon with over 12 years of experience in clinical dentistry. He completed his BDS from the prestigious Sri Aurobindo Institute of Dentistry in 2012 and specializes in painless root canals, smile makeovers, and preventive oral care. Known for his patient-first approach and clear communication, Dr. Ghanghoriya aims to make dental knowledge accessible to everyone. When he’s not in the clinic, he enjoys writing informative dental blogs to help people take better care of their oral health.