Author: Dr. Niraj Ghanghoriya (Dental Specialist) Category: Dental Anatomy & Histology (Student & Pro) Target Audience: Dental Students, Professionals, and Inquisitive Patients Reading Time: ~15 Minutes
Introduction
When we think of a healthy smile, we usually picture white, straight teeth. But as a dental specialist, I often tell my patients: “A house is only as strong as its foundation.” In dentistry, that foundation is the Periodontium.
Beneath the gumline lies a complex, microscopic network of biological “shock absorbers” and “anchors” that keep your teeth stable while allowing them to withstand the massive forces of chewing. Today, we are going deep into the histology of the gums—specifically the periodontal ligament (PDL). Whether you are a dental student preparing for boards or a patient trying to understand why your tooth feels “loose,” this guide covers the microscopic science that makes a massive difference in oral health.
Periodontal Ligament Fibers
The periodontal ligament (PDL) is often misunderstood as just a “glue” that holds the tooth in place. In reality, it is a highly specialized, dynamic connective tissue that acts more like a hammock or a trampoline. It allows the tooth to move microscopically inside the jawbone, dissipating the intense pressure of biting so the bone doesn’t shatter.
At the heart of this system are the periodontal ligament fibers. These are primarily composed of Type I collagen, arranged in specific bundles that connect the cementum (the outer layer of the tooth root) to the alveolar bone.
The “Shock Absorber” Mechanism
In my clinical practice, I often explain to patients who clench their teeth (bruxism) why their teeth might feel sore even if they have no cavities. It is because these fibers are inflamed. When you bite down, your tooth doesn’t just sit there; it is depressed slightly into the socket. The PDL fibers stretch to accommodate this force, transmitting the tension to the bone.
- Tension vs. Compression: Bone is unique; it loves tension but hates compression. The fibers ensure that chewing forces are converted into tension on the bone, which stimulates bone strength. If the tooth were fused directly to the bone (a condition called ankylosis), the bone would resorb over time due to a lack of stimulation.
Clinical Insight: Orthodontics
For my dental student readers, understanding these fibers is the basis of orthodontics. When we put braces on teeth, we are essentially manipulating these fibers. We apply pressure to compress the PDL on one side (causing bone resorption) and stretch it on the other (causing bone deposition). If we move teeth too fast, we risk crushing these fibers and cutting off their blood supply, leading to a process called “hyalinization,” which actually stops tooth movement.
Dr. Niraj’s Clinical Tip: “Healthy PDL fibers are essential for implants too—or rather, the lack of them. Dental implants do not have periodontal ligament fibers; they are fused directly to the bone. This is why I always warn patients that implants have no ‘give’ or ‘sensation’ like natural teeth. You can bite much harder on an implant without knowing it, potentially damaging the crown.”
Periodontal Membrane
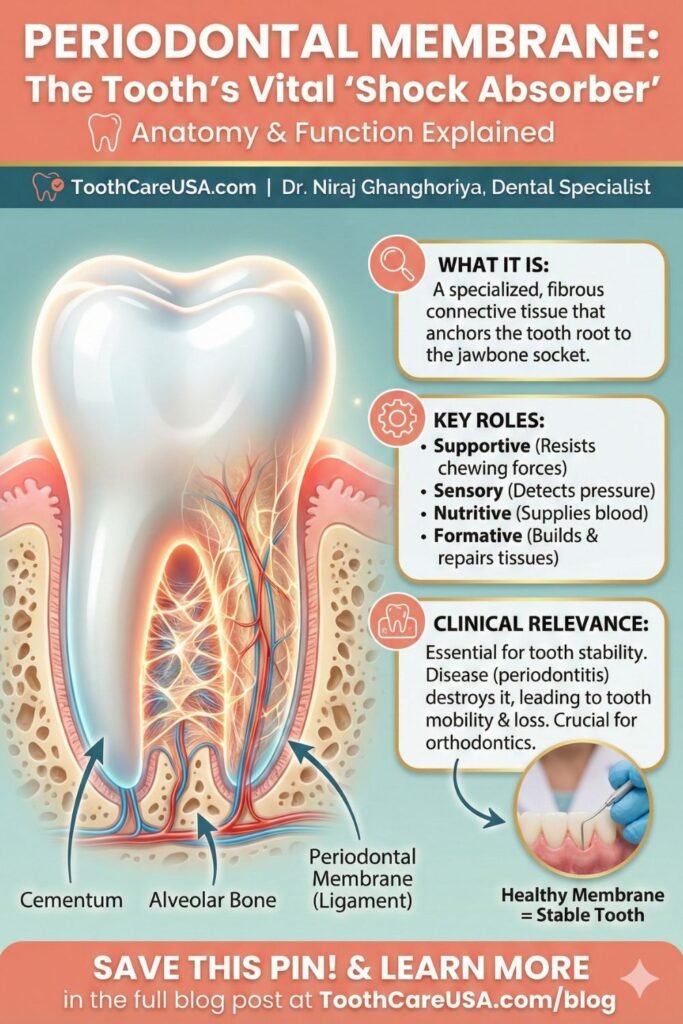
The term “periodontal membrane” is an older, synonymous term for the periodontal ligament, but it often refers specifically to the radiographic space or the physical layer of soft tissue seen between the tooth and bone.
The Space of Life: Width and Function
The average width of the periodontal membrane is approximately 0.2 mm (ranging from 0.15 to 0.38 mm). It is not uniform; it is shaped like an hourglass, being widest at the apex (root tip) and the crest (near the gumline), and narrowest in the middle of the root. This is the fulcrum of rotation for the tooth.
- Age Changes: As we age, the periodontal membrane tends to thin if the tooth is not in heavy function. However, in teeth that carry heavy loads, the membrane can widen.
- Radiographic Importance: When I look at an X-ray, I am looking for the “PDL space”—a thin, dark (radiolucent) line surrounding the root. If this line is thickened, it is a classic sign of trauma, infection, or occlusal trauma (biting too hard).
Proprioception: The Tooth’s “Sense of Touch”
The periodontal membrane is rich in nerve endings. Have you ever wondered how you can feel a tiny stray hair or a grain of sand between your teeth? That is the periodontal membrane at work. It provides proprioception—sensory feedback that tells your brain how hard you are biting and the position of your jaw. Without this membrane, you would constantly fracture your teeth because your jaw muscles wouldn’t know when to stop closing. This sensory input is vital for the “chewing cycle” and protects the entire masticatory system.
Dr. Niraj’s Advice for Patients: “If a tooth feels ‘high’ or touches before the others when you bite, do not ignore it. That sensation is your periodontal membrane warning you that the tooth is receiving too much force. Ignoring it can lead to the widening of the membrane and eventual tooth mobility.”
Periodontal Tissue
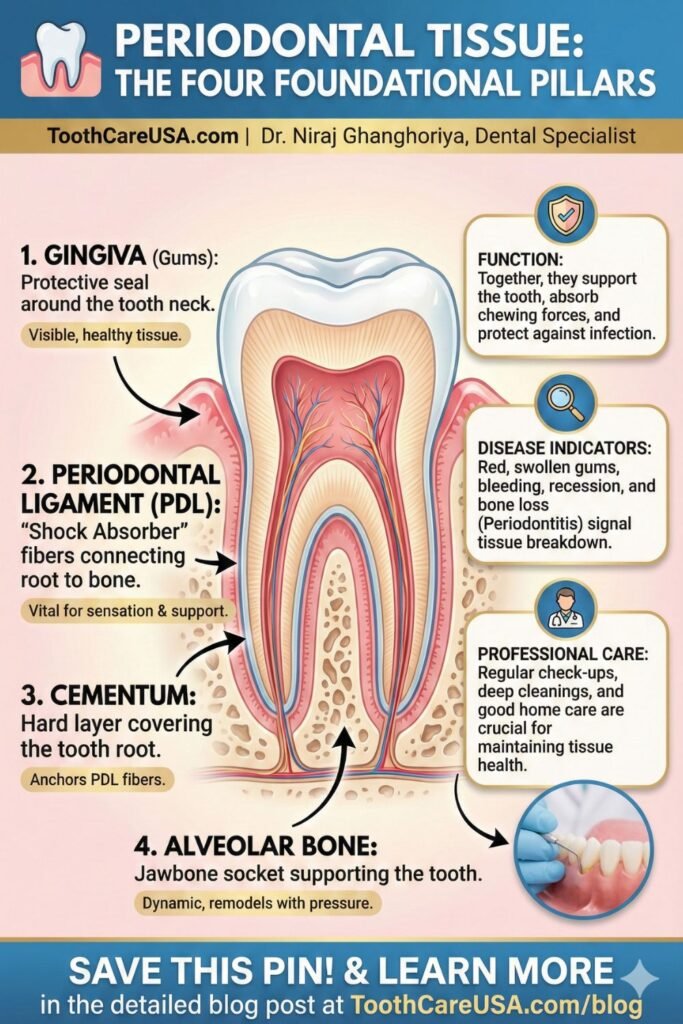
While the ligament is the star of the show, it is just one part of the larger Periodontal Tissue complex, also known as the Periodontium. This system comprises four distinct tissues that must work in perfect harmony.
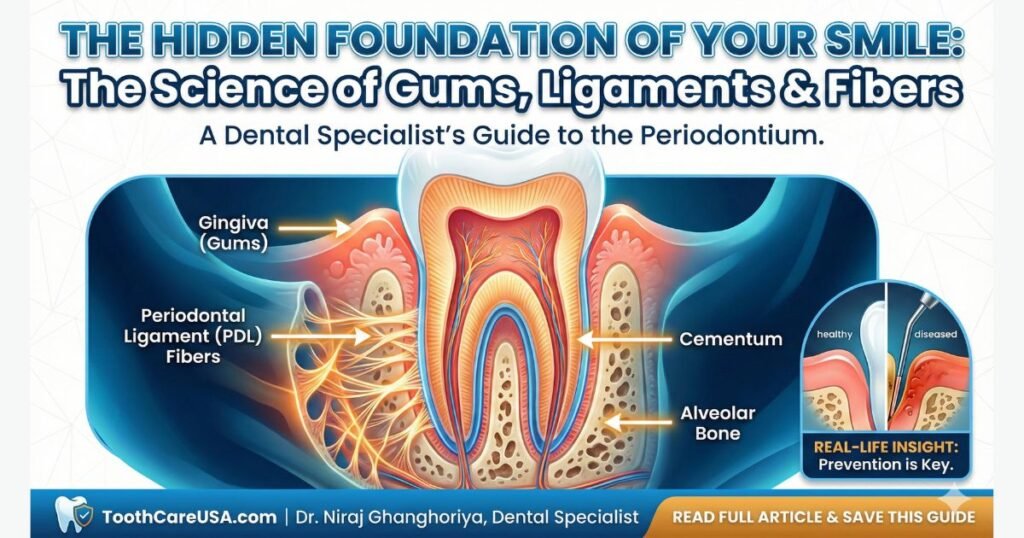
The Four Components of the Periodontium
- Gingiva (Gums): The visible soft tissue that seals the neck of the tooth, protecting the underlying structures from bacteria.
- Periodontal Ligament (PDL): The soft connective tissue attaching the tooth to the bone (our main focus today).
- Cementum: A mineralized layer covering the tooth root. It is softer than enamel and serves as the anchor point for the PDL fibers.
- Alveolar Bone: The specialized part of the jawbone that forms the socket (alveolus) around the tooth.
The Balance of Health vs. Disease
According to the Centers for Disease Control and Prevention (CDC), nearly 47.2% of adults aged 30 years and older in the USA have some form of periodontal disease. This happens when the harmony of these tissues is disrupted. It starts with the gingiva (gingivitis). If left untreated, the inflammation migrates down to the periodontal ligament and alveolar bone. The body, in an attempt to move away from the bacteria, begins to destroy its own bone and fibers. This loss of periodontal tissue is what eventually causes teeth to loosen and fall out.
Regeneration Potential
One of the most exciting areas in periodontics is Guided Tissue Regeneration (GTR). Unlike many other tissues in the body, the periodontal tissue has a unique capacity to regenerate under the right conditions. By using barrier membranes and bone grafts, we can sometimes encourage the body to regrow lost PDL fibers and bone, reversing the damage of gum disease.
Principal Fibers of Periodontal Ligament
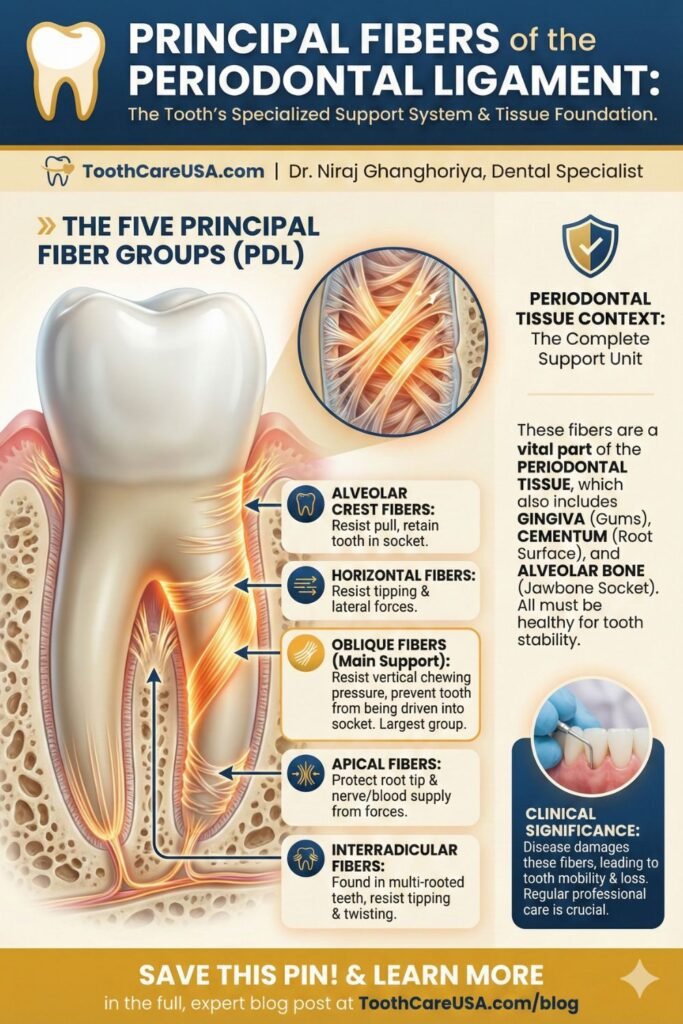
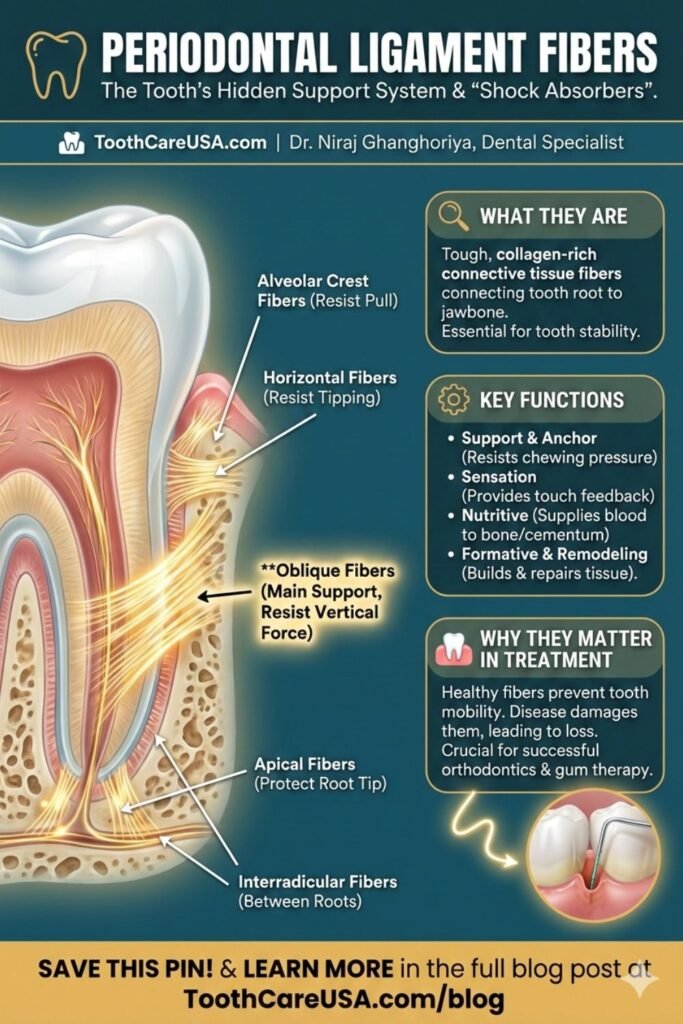
For the dental students and professionals reading this, let’s break down the Principal Fiber Groups. These are the specific bundles of collagen that are named based on their direction and function. They are the “ropes” that hold the ship (tooth) to the dock (bone).
The ends of these fibers that are embedded into the bone and cementum are called Sharpey’s Fibers. They are mineralized, locking the soft tissue firmly into the hard tissue.
1. Alveolar Crest Fibers
- Location: Run diagonally from the cementum just below the CEJ (where crown meets root) to the crest of the alveolar bone.
- Function: They resist extrusive forces (pulling the tooth out) and lateral movements. They are the first line of defense against bacterial invasion.
2. Horizontal Fibers
- Location: Run perpendicular (at a right angle) from the root to the bone.
- Function: Their main job is to resist tipping forces. When you push a tooth with your tongue, these fibers prevent it from tipping over.
3. Oblique Fibers (The Workhorse)
- Location: These are the most abundant fibers. They run diagonally downward from the bone into the cementum.
- Function: They resist vertical masticatory forces. When you bite down, these fibers stretch and suspend the tooth, preventing it from jamming into the bottom of the socket.
4. Apical Fibers
- Location: Radiates from the apex (tip) of the root to the surrounding bone.
- Function: They resist luxation (being pulled out) and protect the delicate blood vessels and nerves entering the root tip.
5. Interradicular Fibers
- Location: Found only in multi-rooted teeth (like molars), running between the roots (the furcation area).
- Function: They resist tipping and twisting (torque) forces.
Dr. Niraj’s Clinical Insight: “When extracting a tooth, I have to sever these fibers. The ‘popping’ sound a patient might hear isn’t bone breaking; it’s often these tough Sharpey’s fibers finally releasing their grip on the bone.”
Cells of the Periodontal Ligament
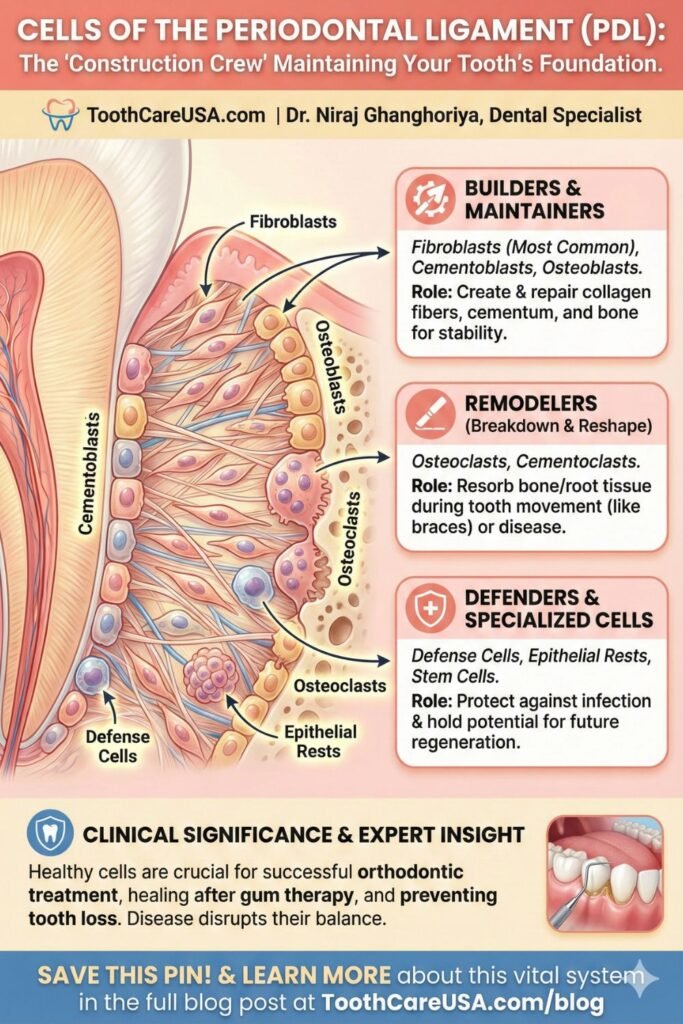
The periodontal ligament is not just inert rope; it is a bustling city of cells. It has a high metabolic rate, meaning it is constantly repairing and replacing itself. If it didn’t, our teeth would fall out from the wear and tear of daily chewing.
1. Fibroblasts: The Architects
- Role: These are the most abundant cells in the PDL. They have a dual function: they synthesize new collagen fibers and degrade old ones.
- Importance: This rapid turnover allows the PDL to adapt to changes. If you start chewing more on the left side, the fibroblasts will beef up the fibers on that side to handle the load.
2. Osteoblasts & Osteoclasts: The Bone Modelers
- Osteoblasts: Build new bone along the socket wall.
- Osteoclasts: Resorb (break down) bone.
- Harmony: These cells work in tandem to reshape the socket during tooth movement (like braces) or physiological drift (natural movement of teeth over time).
3. Cementoblasts: The Anchor Builders
- Role: These cells sit on the surface of the root and produce cementum. Unlike bone, cementum does not remodel easily, which is why orthodontic movement usually resorbs bone rather than the tooth root itself.
4. Epithelial Rests of Malassez
- Role: These are mysterious clusters of cells left over from tooth development (Hertwig’s Epithelial Root Sheath).
- Clinical Danger: While usually dormant, these cells can proliferate when stimulated by inflammation, leading to the formation of dental cysts or tumors in the jaw. This is why we closely monitor any dark spots on X-rays.
5. Defense Cells
- Role: Macrophages, mast cells, and eosinophils patrol the PDL. They are part of the immune system, ready to fight bacteria that breach the gum pocket.
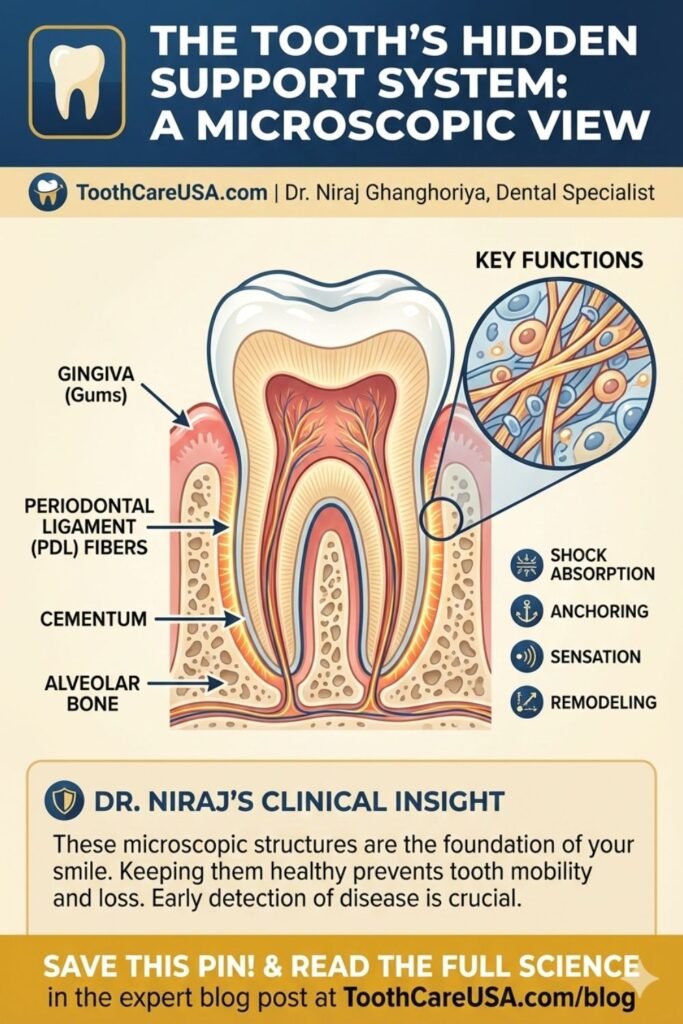
Periodontal Ligament Diagram
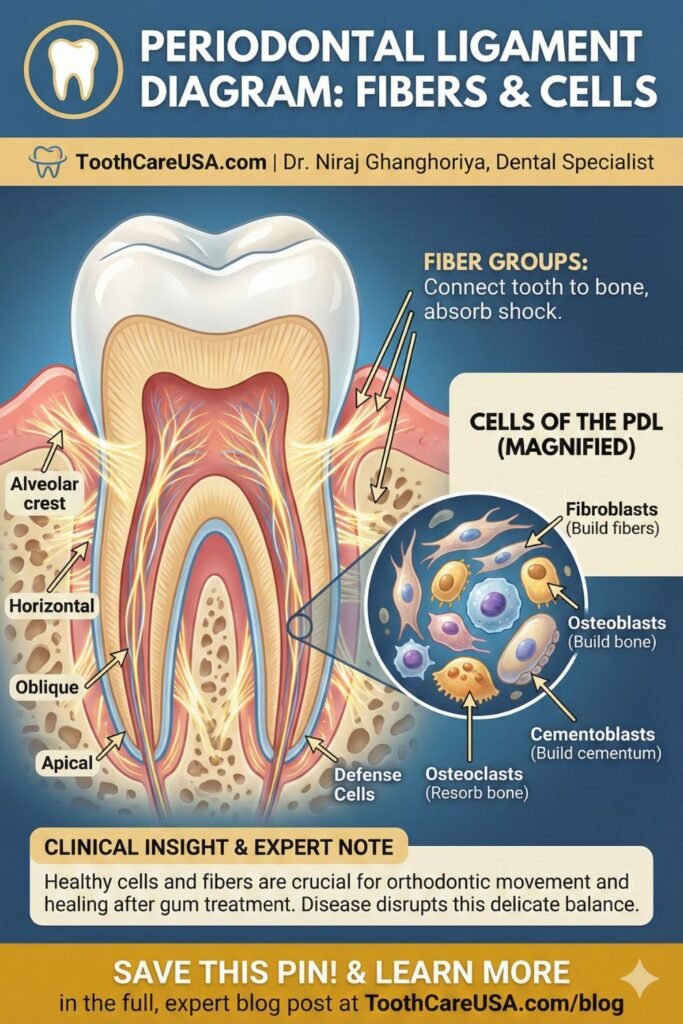
Note: Please refer to the pinned diagram above for a visual breakdown.
Understanding a diagram of the PDL is crucial for visualizing how gum disease progresses. When viewing a cross-section diagram of a tooth, you should look for the following layers from the inside out:
- Pulp: The nerve center.
- Dentin: The main body of the tooth.
- Cementum: The thin outer layer of the root.
- PDL Space: The gap containing the wavy collagen fibers.
- Lamina Dura: The dense, white line of bone lining the socket (critical for X-ray diagnosis).
- Trabecular Bone: The spongy bone supporting the socket.
In a healthy diagram, the Junctional Epithelium (where the gum attaches to the tooth) should be at the CEJ (neck of the tooth). In a disease diagram, you will see this attachment migrate down the root, destroying the PDL fibers in its path. This migration creates a “periodontal pocket,” which is what we measure with a probe during your checkup.
Periodontal Tissue Illustration
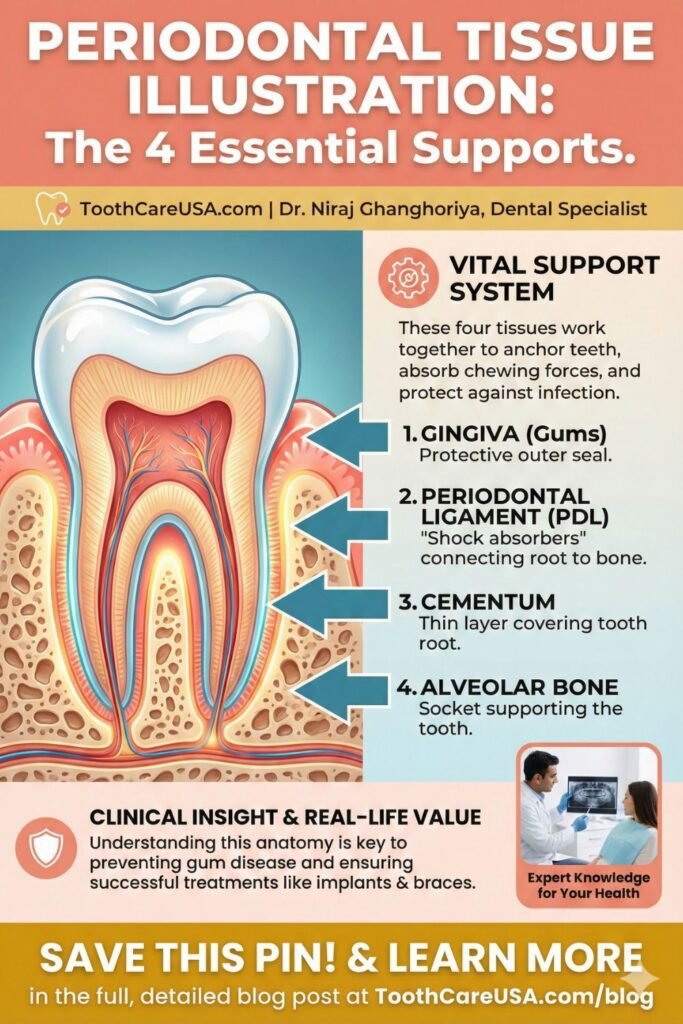
Visualizing the difference between “Gingivitis” and “Periodontitis” is vital for patient education.
Healthy Tissue Illustration
- Color: Coral pink (or pigmented brown/black in darker skin tones).
- Texture: Stippled (like an orange peel).
- Contour: Knife-edged and tight against the tooth.
- Bone Level: High, supporting the neck of the tooth.
Diseased Tissue Illustration (Periodontitis)
- Color: Red, cyan, or purple due to blood stagnation.
- Texture: Smooth, shiny, and swollen (edematous).
- Bleeding: Spontaneous or upon probing.
- Bone Level: Reduced, creating a gap between the gum line and the bone level (attachment loss).
Dr. Niraj’s Takeaway: “Pain is rarely an early sign of periodontal tissue loss. The illustration of disease often looks ‘scary’ with bone loss, but in your mouth, it might just look like a little redness. This is why we call gum disease the ‘silent killer’ of teeth. You cannot rely on a mirror; you need a probe measurement.”
Key Takeaways
- It’s Alive: The Periodontal Ligament is a living, sensing tissue, not just a glue.
- Shock Absorption: The Oblique fibers are the main support against chewing forces.
- Orthodontics: Moving teeth is only possible because of the cellular activity (osteoclasts/osteoblasts) within the PDL.
- Silent Progression: Damage to these fibers and the underlying bone is often painless until it is severe.
- Prevention: Brushing stimulates the gingiva, but only flossing cleans the interdental space where disease starts.
References & Further Reading:
- Carranza’s Clinical Periodontology – Standard textbook for periodontal histology.
- Journal of Periodontology – Research on PDL regeneration.
- CDC Guidelines on Periodontal Disease (2024): Statistics on prevalence in the USA.
- American Academy of Periodontology (perio.org): Patient resources on gum health.
FAQ Section: The Science of Your Gums and Periodontal Ligament Fibers
Can periodontal ligament fibers regenerate after gum disease?
Yes, but only with specific treatment. Once destroyed by periodontitis, these fibers do not regrow naturally on their own. However, in my practice, we can often restore them using Guided Tissue Regeneration (GTR). This procedure uses barrier membranes and bone grafts to stimulate the body to rebuild the lost ligament and bone.
Do dental implants have a periodontal ligament?
No, dental implants do not have a periodontal ligament. They fuse directly to the jawbone in a process called osseointegration. Because they lack this “shock absorber,” implants have no sensation of pressure. I always advise patients to be careful not to bite too hard on implants, as they cannot feel stress like natural teeth can.
Why do my teeth feel loose when I have braces?
Teeth feel loose during orthodontics because the braces are actively remodeling the periodontal ligament. The pressure stretches the fibers and temporarily widens the ligament space, allowing the tooth to move through the bone. This mobility is normal and necessary; once the movement stops, the fibers re-tighten, and the tooth stabilizes.
What is the difference between the gingiva and the periodontal ligament?
The gingiva (gum) is the visible pink tissue that covers the bone and protects the tooth neck, while the periodontal ligament is the internal connective tissue hidden below the gumline. Think of the gingiva as the “skin” that seals out bacteria, and the ligament as the “anchor” that physically locks the tooth root to the jawbone.
What happens if the periodontal ligament is damaged by trauma?
If a tooth is hit hard, the periodontal ligament can become inflamed, causing the tooth to feel “high” or sore when biting. In severe cases (avulsion), if the fibers dry out, the tooth cannot be replanted successfully. If you knock out a tooth, keep it moist in milk or saliva to keep these vital cells alive until you reach the dentist.
About the Author: Dr. Niraj Ghanghoriya is a Dental Specialist and the founder of ToothCareUSA.com. He is dedicated to providing evidence-based, easy-to-understand dental education to patients across the USA.
Disclaimer: This article is for educational purposes only and does not constitute medical advice. Always consult with your dental professional for diagnosis and treatment.
Periodontal Disease: Your Comprehensive Resource
I invite you to read the articles below for a complete breakdown of gum disease causes, clinical treatments, and my recommended home care routines.
Dental Implant Cost Chicago: The 2026 Price Guide & Hidden Fees S1A5
Author: Dr. Niraj Ghanghoriya (Dental Specialist) Micro-Note: Educational purposes only. See full disclaimer below. Quick…
The Real Cost of Dental Implants in Indiana: A Specialist’s Transparent Guide (2026) S1A4
By Dr. Niraj Ghanghoriya (Dental Specialist).Educational purposes only. See full disclaimer below. Quick Answer: What…
Price for Mini Dental Implants (2026 Cost Guide & Fee Breakdown) S1A3
Author: Dr. Niraj Ghanghoriya, (Dental Specialist), Educational purposes only. See full medical disclaimer below. Quick…
The Cost of Zirconia Implants: Why ‘Cheap’ Ceramic Can Cost You Your Bone
Dr. Niraj’s Quick Answer (2026 Estimate) In the US, Cost of Zirconia Implants(single) lies between…
Bolsa Periodontal: A Multilingual Guide to Gum Care,Bolsa Periodontal(Global Periodontal Health)(Blog 6)
Author: Dr. Niraj Ghanghoriya (Dental Specialist) | Website: ToothCareUSA.com Category: Global Periodontology (International Resources) Introduction…
Decoding the Dentist’s Code: Understanding Periodontal Instruments & periodontal chart (Blog 5)
By Dr. Niraj Ghanghoriya, Dental Specialist | ToothCareUSA.com Key Takeaways: The “Numbers”: Hearing “3, 2,…

Dr. Niraj Ghanghoriya is a passionate dental surgeon with over 12 years of experience in clinical dentistry. He completed his BDS from the prestigious Sri Aurobindo Institute of Dentistry in 2012 and specializes in painless root canals, smile makeovers, and preventive oral care. Known for his patient-first approach and clear communication, Dr. Ghanghoriya aims to make dental knowledge accessible to everyone. When he’s not in the clinic, he enjoys writing informative dental blogs to help people take better care of their oral health.