By Dr. Niraj Ghanghoriya, Dental Specialist | ToothCareUSA.com
Key Takeaways:
- The “Numbers”: Hearing “3, 2, 3” is a good sign; numbers above 4 indicate potential gum disease.
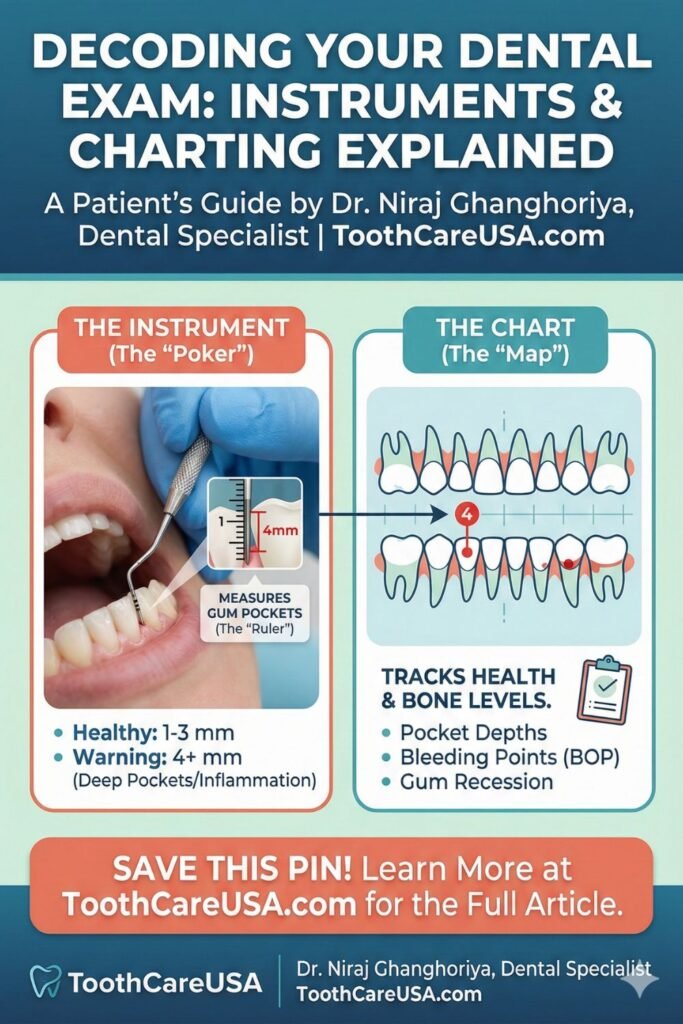
- The “Poker”: The instrument used is a periodontal probe, and it acts as a ruler, not a needle.
- Early Detection: Regular charting is the only way to catch “silent” gum disease before bone loss occurs.
- Accuracy Matters: We use specific probes and charts to create a roadmap of your oral foundation.
Have you ever sat in the dental chair, listening to your hygienist call out a string of numbers like “3, 2, 3… 4, 3, 2” while I or another clinician writes them down? For many patients, this part of the visit feels like a secret code. You might feel a gentle poking sensation, hear some technical jargon, and wonder, “Is that bad? Did I fail the test?”
As a dental specialist, I want to pull back the curtain on this process. We aren’t just counting teeth; we are measuring the very foundation that holds them in place. This guide will walk you through the tools we use and the charts we create to ensure your smile lasts a lifetime.
Periodontal Chart
A periodontal chart is essentially the map of your mouth. Think of your teeth like houses; the periodontal chart is the survey of the land those houses are built on. In my practice at ToothCareUSA, I often tell patients that we can have the strongest, cleanest “house” (tooth), but if the “land” (gum and bone) is eroding, the house will eventually fall.
The periodontal chart is a graphic and numeric record that documents the health of the gingiva (gums) and the bone support for every single tooth. It is a legal medical record that tracks changes over time. When you visit us for your routine cleaning, we aren’t just cleaning; we are comparing today’s map to the map from six months ago.
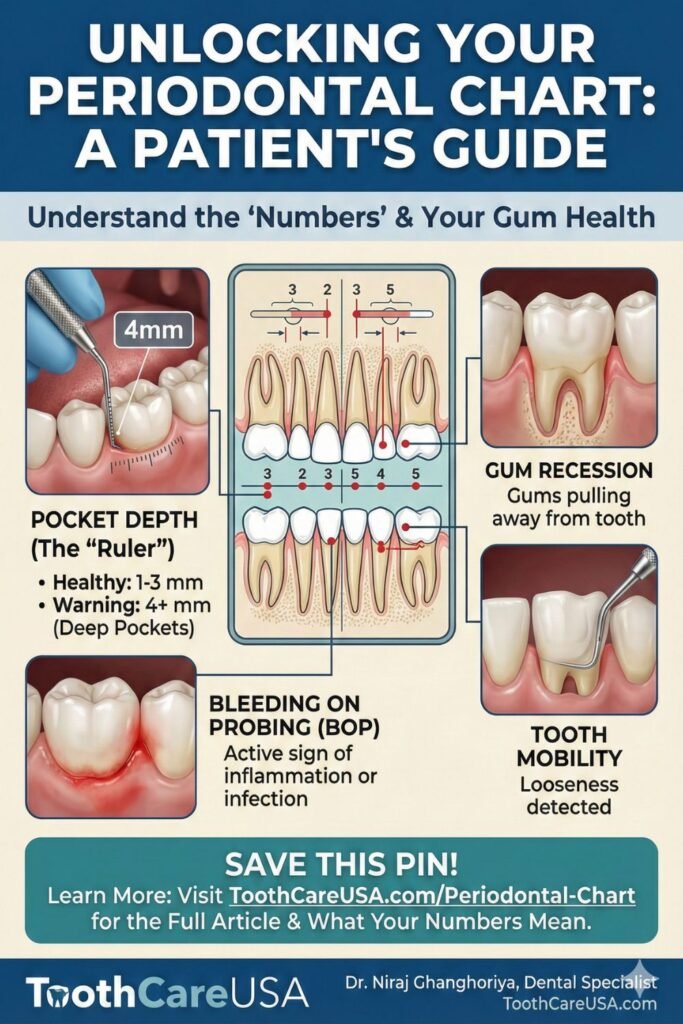
What exactly goes onto a Periodontal Chart?
A comprehensive chart tracks several critical data points:
- Pocket Depths: These are the millimeter measurements you hear us reading aloud. They measure the space between the gum and the tooth.
- Bleeding Points: We note specific sites that bleed upon gentle touching. Bleeding is never normal; it is the body’s distress signal indicating active infection or inflammation.
- Recession: These notes indicate that the gum line has migrated down the root of the tooth, exposing sensitive surfaces.
- Furcation Involvement: For multi-rooted teeth (molars), we chart if bone loss has occurred between the roots.
- Mobility: We literally wiggle the tooth to see if it is loose, grading it on a scale of I to III.
According to the Centers for Disease Control and Prevention (CDC), nearly 47.2% of American adults aged 30 years and older have some form of periodontal disease. Without a detailed periodontal chart, this disease is invisible. The chart allows us to diagnose “silent” bone loss before a patient ever feels pain. By the time a tooth hurts or feels loose, it is often too late to save it. The chart is our early warning system.
Dr. Niraj’s Clinical Insight: “Don’t be afraid to ask to see your chart! I love showing patients their ‘map.’ If you see a lot of red ink (indicating bleeding) or numbers above 4mm, don’t panic. It’s simply data that tells us exactly where we need to focus our efforts. A chart isn’t a judgment of your brushing; it’s a tool for your health.”
Periodontal Probe
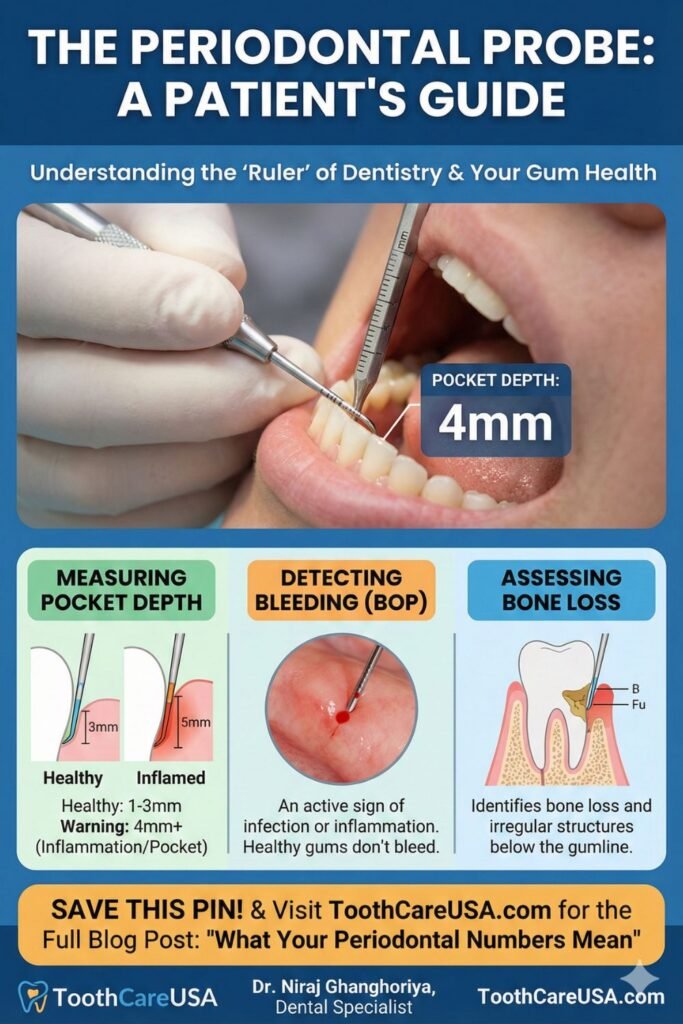
The instrument responsible for those numbers is the periodontal probe. I often jokingly refer to this as the “dental dipstick” or a tiny ruler. It is perhaps the most critical diagnostic tool in a dental specialist’s arsenal.
Patients often mistake the probe for the “explorer” (the sharp hook used to check for cavities). However, a periodontal probe is different. It has a blunt, rounded tip and is marked with millimeter increments—usually black bands that make it easy for the clinician to read.
How does it work?
The probe is gently inserted into the sulcus, which is the natural space between your tooth and the surrounding gum tissue. In a healthy state, this space is shallow, like a turtleneck sweater fitting snugly around a neck. The probe slides in, hits the bottom of the pocket (the attachment level), and we read the depth.
- 1-3 mm: This is the “Green Zone.” The gums are tight and healthy, and you can easily clean this space with a toothbrush and floss.
- 4-5 mm: This is the “Yellow Zone.” The measurement indicates inflammation or early bone loss. You cannot clean this deep with floss; bacteria are thriving at the bottom of this pocket.
- 6 mm and above: This is the “Red Zone.” This indicates advanced periodontal disease. At this depth, the gum has detached significantly from the tooth, and professional intervention is mandatory to stop tooth loss.
Many patients ask, “Why does it hurt when you do this?” In a strictly healthy mouth, probing should be painless—perhaps a slight pressure, but not pain. If you feel sharp pain during probing, it is usually because the gum tissue is inflamed and ulcerated on the inside (think of it like touching an open wound on your skin). The pain is actually a symptom of the disease, not a fault of the instrument.
Dr. Niraj’s Advice: “If you feel tenderness during probing, let your hygienist know, but try to stay relaxed. Tensing up makes the muscles tight and the experience more uncomfortable. Remember, the probe is diagnostic. We aren’t poking to hurt you; we are measuring to heal you.”
Periodontal Charting
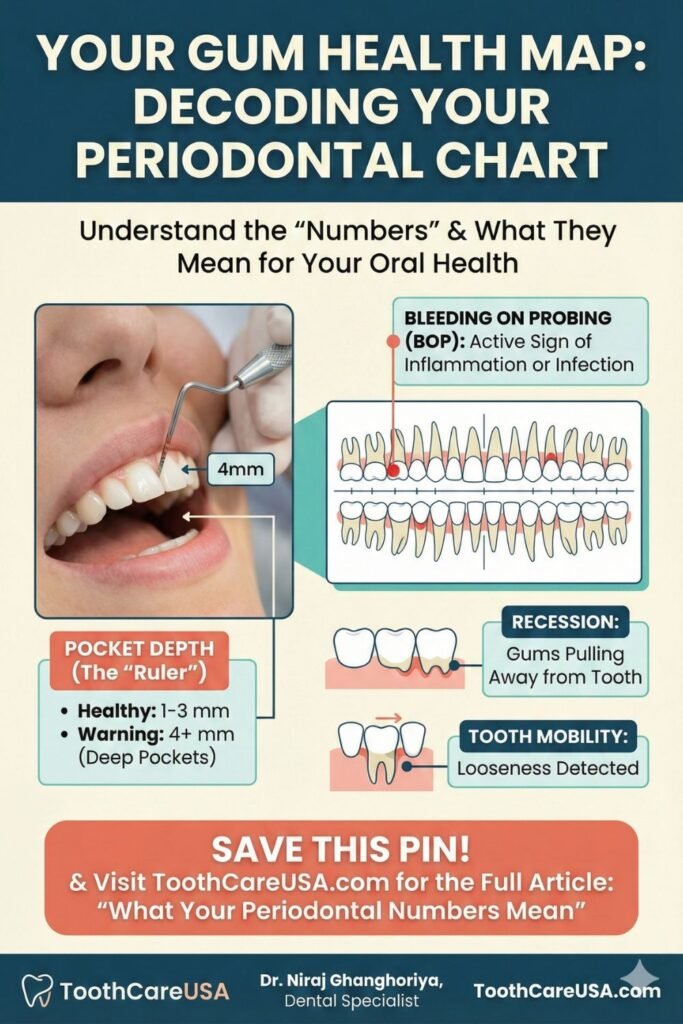
Periodontal charting is the active process of gathering the data. It is a systematic investigation of your oral health. When we perform periodontal charting at ToothCareUSA, we are typically measuring six specific points on every single tooth: three on the cheek side (distal, buccal, mesial) and three on the tongue side (distal, lingual, mesial).
If you have a full set of 28 teeth (excluding wisdom teeth), that is 168 separate measurements we take in a matter of minutes!
The “Periodontal Experience” in the Chair During charting, you play an active role. We need you to remain open and still. As we call out the numbers for the assistant (or computer) to record, you are hearing a real-time report card of your mouth.
- The Sound of Health: A rhythmic “2, 3, 2… 3, 2, 3.”
- The Sound of Infection: “5, 5, bleeding… 6, 4, bleeding… 7 with mobility.”
Why is accurate charting vital? Periodontal disease is site-specific. You can have perfect health on the upper right molars and severe, active disease on the lower front teeth. Generalized X-rays show us bone levels, but they are 2D images of 3D objects. X-rays often hide early bone loss. Periodontal charting is the only way to verify the true attachment level of the gum to the tooth.
We also use charting to determine your ASA Case Type (American Society of Anesthesiologists classification for dental patients) and your periodontal stage (Stage I through IV). This determination dictates whether you need a “regular cleaning” (prophylaxis) or a “deep cleaning” (scaling and root planing). Insurance companies in the US specifically require this charting data to authorize payment for treatment. Without a chart showing pockets of 4mm or greater, they will often deny claims for gum therapy.
Clinical Tip: “I recommend a full periodontal chart once a year for all adult patients. If you have a history of gum disease, we may spot-check specific deep areas every 3 to 4 months. If your dentist hasn’t measured your gums in over a year, ask for it! It is the standard of care.”
Periodontal Instruments
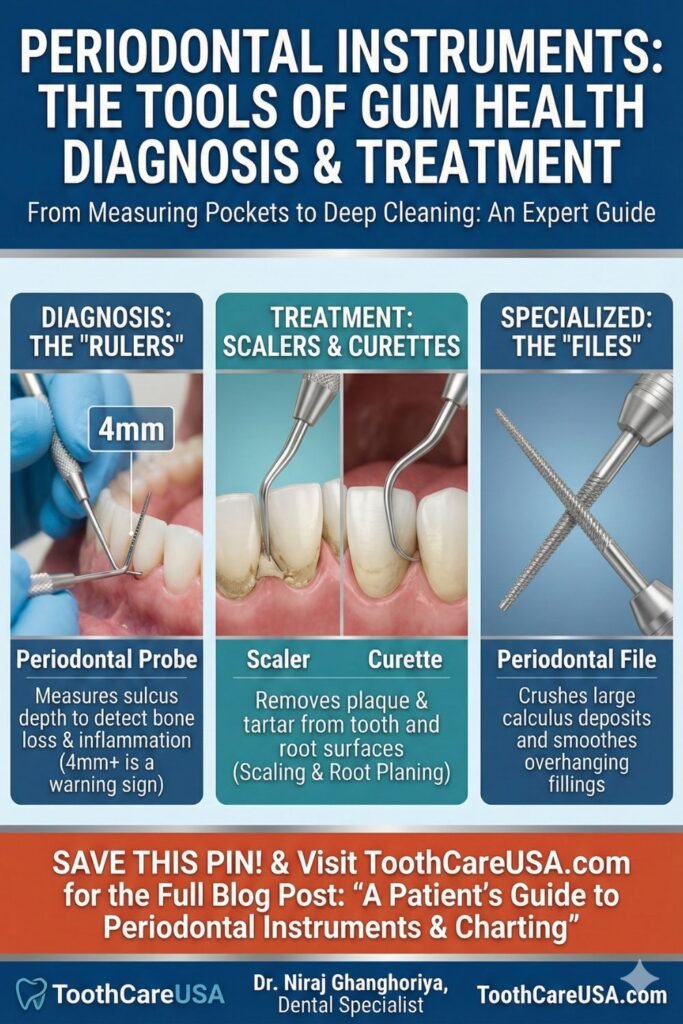
While the probe is for looking, other periodontal instruments are for doing. When we move from diagnosis to treatment (therapy), the tray setup changes. Understanding these tools helps alleviate the anxiety of the “scraping” sounds you hear during a cleaning.
The Periodontal Tray Set Up.
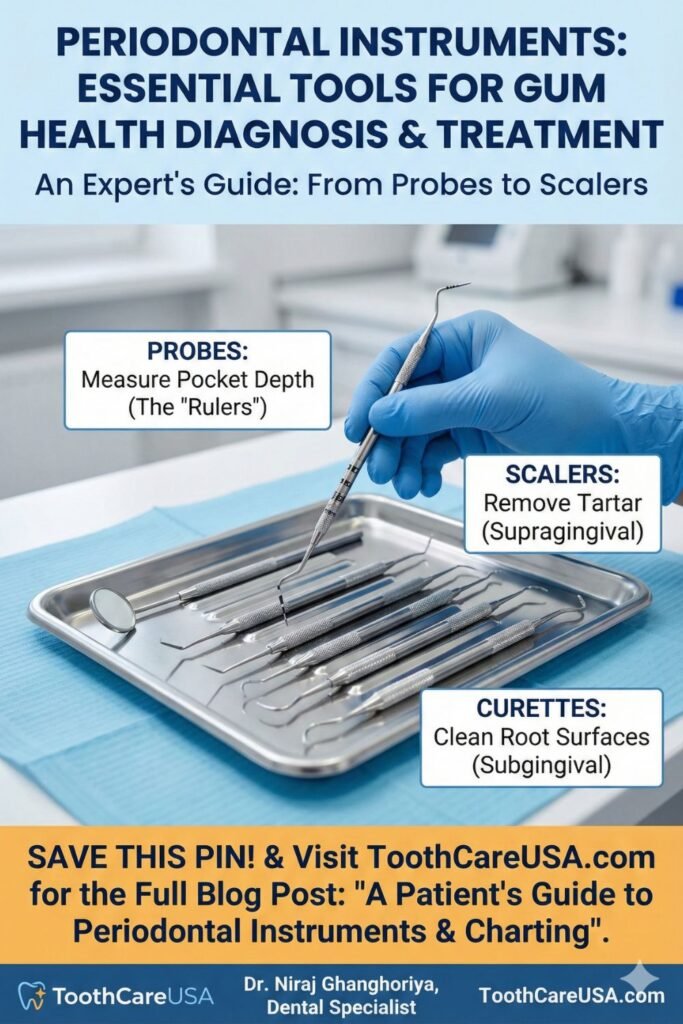
A standard tray for a dental hygienist or specialist usually includes:
- Mirror: For retraction and vision.
- Probe/Explorer: For finding calculus (tartar) and measuring pockets.
- Scalers & Curettes: These are the workhorses.
- Scalers (like the Sickle Scaler) have a pointed tip and are used to snap off heavy tartar above the gum line.
- Curettes (like the Gracey Curette) have a rounded tip and are designed to go below the gum line to smooth the root surface without damaging the soft tissue.
The Periodontal File.
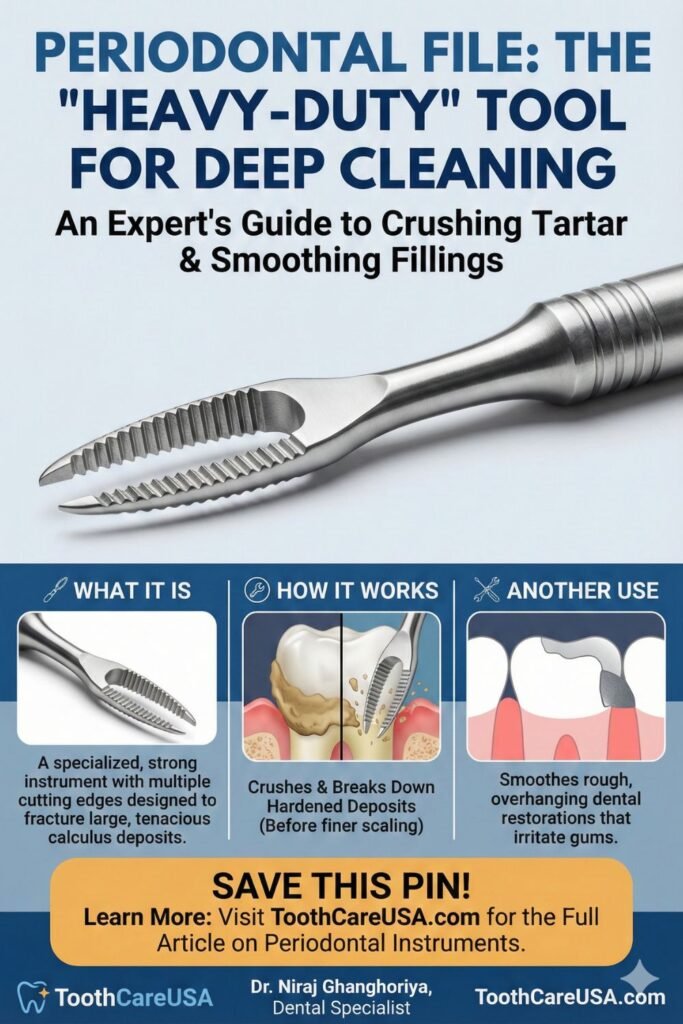
The Periodontal File: The “Heavy-Duty” Crusher
While the periodontal probe is the “ruler” and the curette is the “cleaner,” the periodontal file is the “crusher.” This is a specialized instrument that many patients hear before they feel. If you have ever heard a distinct “crunching” sound during a deep cleaning, we were likely using this tool.
What is a Periodontal File? Unlike a scaler, which has a single blade, a periodontal file has a series of multiple cutting edges lined up on a flat base—almost like a tiny, surgical-grade cheese grater. It is designed for strength and leverage.
Why Do We Use It? In my practice at ToothCareUSA, I reach for a periodontal file in two specific scenarios where standard instruments might fail:
- Crushing Tenacious Calculus: When tartar (calculus) stays on the root for a long time, it calcifies and becomes as hard as concrete. A regular scaler might slip over it, burnishing the surface (making it smooth but still infected). The periodontal file allows me to fracture and crush these large “icebergs” of calculus so they can be easily removed.
- Smoothing Overhanging Fillings: Sometimes, an old filling might stick out too far (an “overhang”), trapping food and bacteria against the gum. As shown in the infographic above, I use the file to shave down that rough edge, smoothing the restoration so your gums can heal properly.
Dr. Niraj’s Clinical Insight: “Don’t be alarmed by the ‘heavy-duty’ description. While the periodontal file is strong, it is used with great control. We use it to prepare the tooth surface, breaking up the heavy deposits so we can finish with fine hand scaling for a perfectly smooth root.”
Ultrasonic Instruments In periodontics
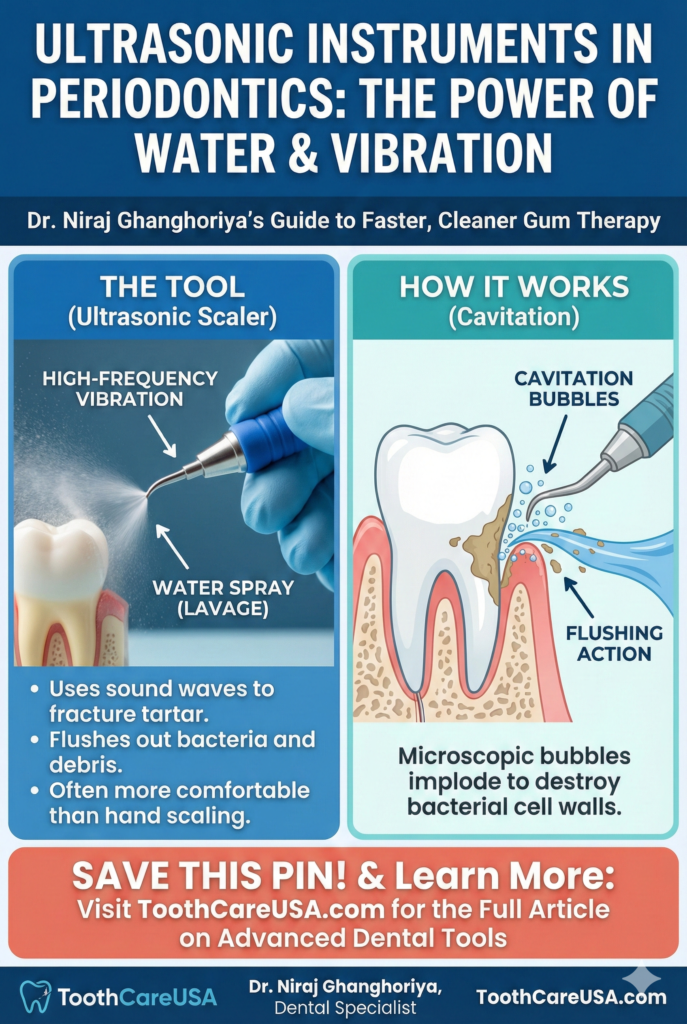
Modern periodontics also relies heavily on ultrasonic scalers (like the Cavitron). These use high-frequency vibration and water to blast away tartar and flush out bacteria. They are often more comfortable than hand instruments and are highly effective at disrupting the “biofilm” (bacterial colonies) that causes gum disease.
Dr. Niraj’s Insight: “Many patients hate the sound of the scraping. I get it—it sounds like nails on a chalkboard! But that sound is actually the sound of success. It means we are removing the calcified bacteria that your toothbrush can’t budge. If we leave that tartar there, your immune system will destroy your bone trying to get away from it.”
Basic Periodontal Examination
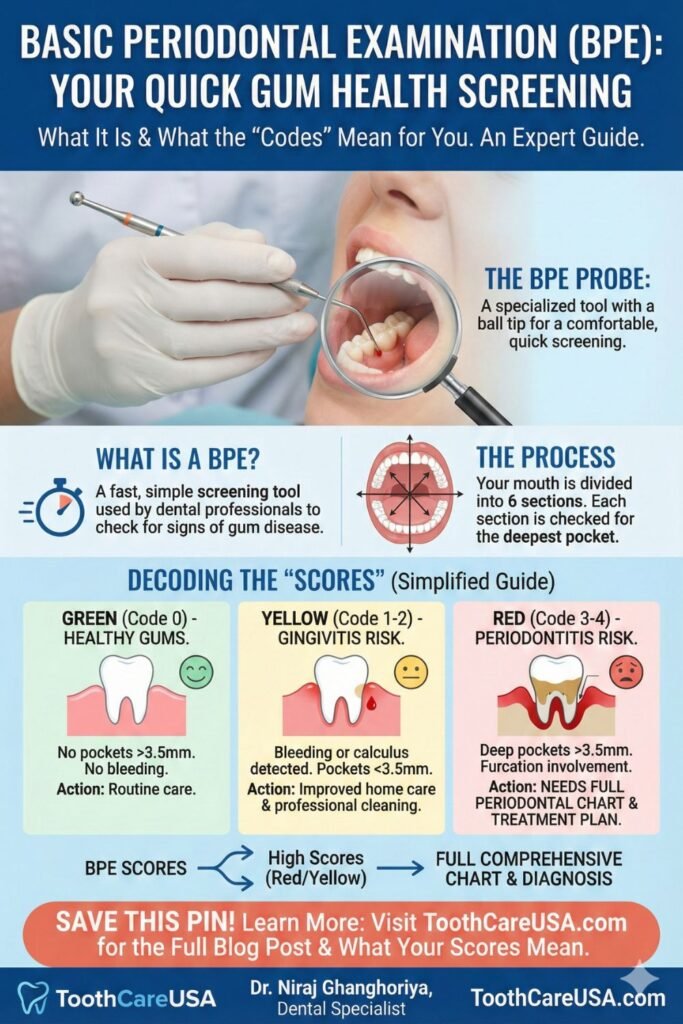
Not every patient needs a full, time-consuming 168-point chart at every single visit. This is where the Basic Periodontal Examination (BPE)—often referred to in the US as the Periodontal Screening and Recording (PSR)—comes into play.
What is the BPE/PSR?
This is a rapid screening tool. Instead of measuring every single millimeter on every tooth, we divide the mouth into six sextants (Upper Right, Upper Front, Upper Left, etc.). We walk the probe around the teeth in that section and record only the highest score for that entire section using a simplified code (0 to 4).
- Code 0: Perfect health.
- Code 1: Bleeding, but no pockets. (Needs better brushing/flossing).
- Code 2: Calculus present, but no deep pockets. (Needs professional cleaning).
- Code 3: Pockets of 3.5mm to 5.5mm. (Needs comprehensive charting and likely treatment).
- Code 4: Pockets deeper than 5.5mm. (Serious condition requiring specialist care).
Why do we use it?
The BPE/PSR is efficient. For a teenager or a healthy young adult, it allows us to verify health quickly without putting them through a long charting process. However, if we find a “Code 3” or “Code 4” in any section, we stop the screening and switch immediately to a full Periodontal Chart for that area.
In my practice, I view the BPE/PSR as a triage system. It helps us identify who is healthy, who has gingivitis (reversible gum inflammation), and who has periodontitis (irreversible bone loss).
Dr. Niraj’s Advice: “The BPE/PSR is a great screening tool, but it has limits. It doesn’t always show the full picture of bone recession. If you are over 40 or a smoker, I almost always prefer the full chart over the screening to ensure we don’t miss anything.”
Types of Periodontal Probes
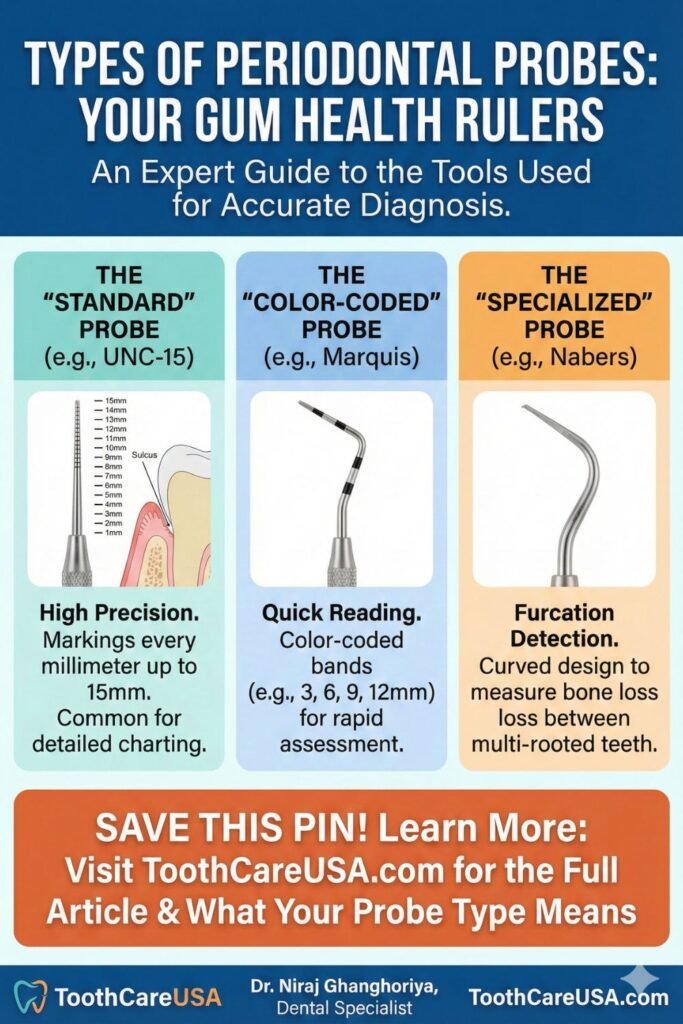
You might think a ruler is a ruler, but in dentistry, precision is everything. There are several types of periodontal probes, and the one I choose depends on the specific anatomy of the patient’s teeth and the severity of their disease.
1. The UNC-15 Probe (University of North Carolina). This is the gold standard for clinical research and specialists. It has markings for every single millimeter up to 15mm. It is slightly thicker but allows for extreme accuracy. If I need to know if a pocket is 4mm or 5mm to decide on surgery, this is the probe I use.
2. The Marquis Probe This is a color-coded probe. It usually has alternating silver and black bands every 3mm (3, 6, 9, 12). It is very easy to read visually. It is great for general screenings where we need to quickly see if a pocket is in the “danger zone” (past the first 3mm band).
3. The Nabers Probe This looks very different—it is curved, not straight. We use the Nabers probe specifically to measure furcation involvement. On multi-rooted teeth (like molars), gum disease can eat the bone away between the roots. The curved Nabers probe allows me to hook between the roots to see if the tunnel goes all the way through. This is a critical measurement for determining the long-term prognosis of a tooth.
4. Plastic Probes We use these specific probes when checking dental implants. Titanium implants can scratch easily, and scratching them creates a rough surface where bacteria can hide. Therefore, we use flexible plastic instruments to gently check the health of implants without damaging their delicate surface.
Dr. Niraj’s Clinical Insight: “The type of probe matters less than the skill of the hand using it. Successful probing requires a tactile sense—a ‘feel’ for the tissue. It is an art form as much as a scientific measurement.”
References & Further Reading
- American Academy of Periodontology (AAP): Gum Disease Information for Patients.
- Centers for Disease Control and Prevention (CDC): Periodontal Disease Facts & Statistics.
- American Dental Association (ADA): MouthHealthy.org – Periodontal Charting.
Disclaimer: This content is for educational purposes only and does not constitute medical advice. Always consult with your dentist or periodontist for a professional diagnosis.
FAQ On Periodontal Instruments & Periodontal Chart
What do the numbers my dentist calls out mean?
The numbers represent the depth of the space (pocket) between your tooth and gum in millimeters. In my clinical practice, I explain that 1 to 3 mm indicates healthy gums. Any number 4 mm or higher suggests inflammation or gum disease, meaning bacteria are trapped deeper than your toothbrush or floss can reach.
Is periodontal probing supposed to be painful?
Periodontal probing should be painless, though you may feel slight pressure. If you experience sharp pain or significant discomfort, it is usually a sign that your gum tissue is inflamed and ulcerated from infection. As we treat the gum disease and health returns, these exams will become comfortable and pain-free.
What is considered a “bad” gum pocket depth?
A measurement of 4 mm is the critical tipping point where gum disease begins. While 1-3 mm is healthy, pockets of 5 mm or deeper indicate moderate to severe periodontitis involving permanent bone loss. At ToothCareUSA, we treat any pocket 5 mm or greater as an active infection requiring professional intervention immediately.
Why do my gums bleed during the charting exam?
Healthy gums do not bleed, even when touched by dental instruments. Bleeding on probing (BOP) is the body’s active “alarm system” signaling infection or gingivitis. It is not caused by the probe injuring you, but rather by the fragility of the infected tissue reacting to the diagnostic touch.
Can deep gum pockets heal on their own?
Deep pockets caused by bone loss (periodontitis) cannot heal without professional treatment. While you can reverse gingivitis (surface inflammation) at home, pockets deeper than 4 mm contain hardened tartar that must be removed by a dental professional. Once cleaned, the gums can tighten, and the pocket depth will often decrease.
Periodontal Disease: Your Comprehensive Resource
I invite you to read the articles below for a complete breakdown of gum disease causes, clinical treatments, and my recommended home care routines.
Dental Implant Cost Chicago: The 2026 Price Guide & Hidden Fees S1A5
Author: Dr. Niraj Ghanghoriya (Dental Specialist) Micro-Note: Educational purposes only. See full disclaimer below. Quick…
The Real Cost of Dental Implants in Indiana: A Specialist’s Transparent Guide (2026) S1A4
By Dr. Niraj Ghanghoriya (Dental Specialist).Educational purposes only. See full disclaimer below. Quick Answer: What…
Price for Mini Dental Implants (2026 Cost Guide & Fee Breakdown) S1A3
Author: Dr. Niraj Ghanghoriya, (Dental Specialist), Educational purposes only. See full medical disclaimer below. Quick…
The Cost of Zirconia Implants: Why ‘Cheap’ Ceramic Can Cost You Your Bone
Dr. Niraj’s Quick Answer (2026 Estimate) In the US, Cost of Zirconia Implants(single) lies between…
Bolsa Periodontal: A Multilingual Guide to Gum Care,Bolsa Periodontal(Global Periodontal Health)(Blog 6)
Author: Dr. Niraj Ghanghoriya (Dental Specialist) | Website: ToothCareUSA.com Category: Global Periodontology (International Resources) Introduction…
Decoding the Dentist’s Code: Understanding Periodontal Instruments & periodontal chart (Blog 5)
By Dr. Niraj Ghanghoriya, Dental Specialist | ToothCareUSA.com Key Takeaways: The “Numbers”: Hearing “3, 2,…

Dr. Niraj Ghanghoriya is a passionate dental surgeon with over 12 years of experience in clinical dentistry. He completed his BDS from the prestigious Sri Aurobindo Institute of Dentistry in 2012 and specializes in painless root canals, smile makeovers, and preventive oral care. Known for his patient-first approach and clear communication, Dr. Ghanghoriya aims to make dental knowledge accessible to everyone. When he’s not in the clinic, he enjoys writing informative dental blogs to help people take better care of their oral health.